まとめと対策

携帯電話による健康への影響を示した研究は数多く、普及度から考えて現在の人々の健康に及ぼしている影響は非常に大きいものと考えられます。
そして若い人ほど電磁波に脆弱であるため、妊娠中の女性や未成年者、妊活中やその予定の有る方は、携帯電話の利用は控えるべきといえます。
電磁波による健康への影響は主として活性酸素の増加に起因しているため、抗酸化作用のある食品の摂取に努めることで、ある程度の軽減は可能であると考えられます。
目次All_Pages
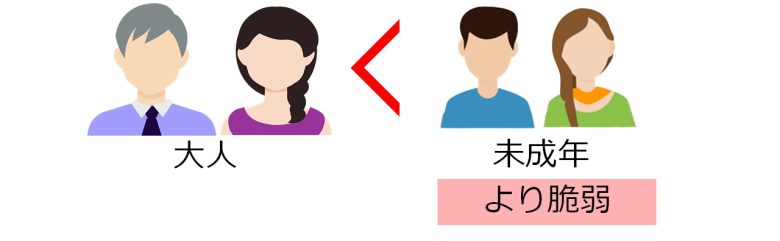
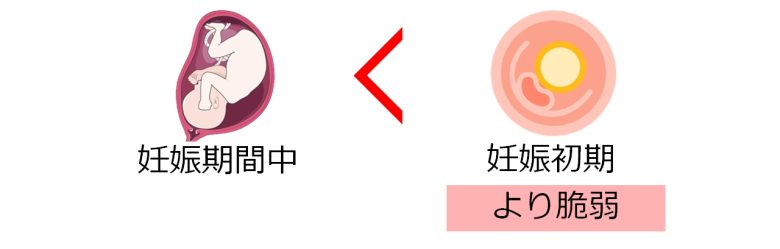
若い人ほど電磁波に脆弱
今回紹介した研究でのポイントは、胎児や乳幼児や子ども、青年など、若い人ほど電磁波に脆弱ということです。
若い人ほど電磁波に脆弱な証拠
未成年はより脆弱
スウェーデン全土の18歳以上の膠芽腫患者の方について、発症までの携帯電話の利用年数が長くなるほど、生存率が低下しました。(Carlberg and Hardell 2014)
この研究では、大人になってからの携帯・コードレス電話の初使用より、未成年からの初使用の方が、生存率がより低下しました。(Carlberg and Hardell 2014)
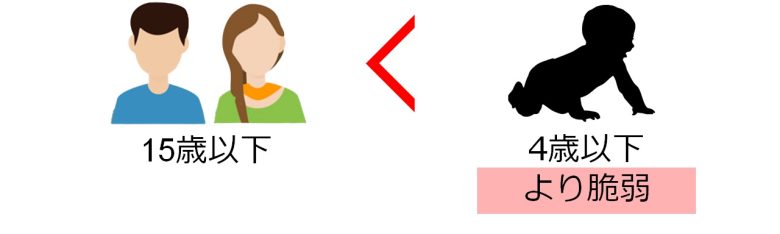
乳幼児はより脆弱
旧西ドイツ全土の15歳以下の子どもについて、夜間の寝室の低周波電磁波が強くなるほど、急性白血病が増加しました。 (Schüz et al. 2001)
この研究では、15歳以下の子どもより、4歳以下の乳幼児の方が、白血病の増加度 (オッズ比) がより大きくなりました。(Schüz et al. 2001)
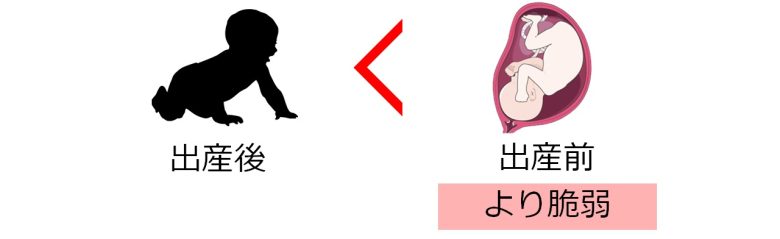
胎児はより脆弱
デンマーク全土から募った妊娠中の研究参加者について、出産前後に携帯電話を利用していると、生まれた子どもが7歳の時に問題行動が増加しました。(Divan et al. 2008)
この研究では、出産後より、出産前の電磁波被曝の方が、問題行動の増加度 (オッズ比) がより大きくなりました。(Divan et al. 2008)
胚はより脆弱
スウェーデン全土の妊娠中の従業員について、ビデオ表示端末 (VDT)を仕事で利用していると、赤ちゃんの先天異常が増加しました。(Ericson and Källén 1986)
この研究では、利用期間が妊娠初期の頃を含む場合、先天異常の増加度 (オッズ比) がより大きくなりました。(Ericson and Källén 1986)
若い人ほど電磁波に脆弱な理由
仕組みの面からいってもこれは裏付けられます。
電磁波は活性酸素を増加させてDNAなどを損傷するということが示されていますが、これは特に増殖中の細胞にとって有害です。
なぜならDNAが損傷したままDNAが複製されると、突然変異や細胞死が発生するためです。
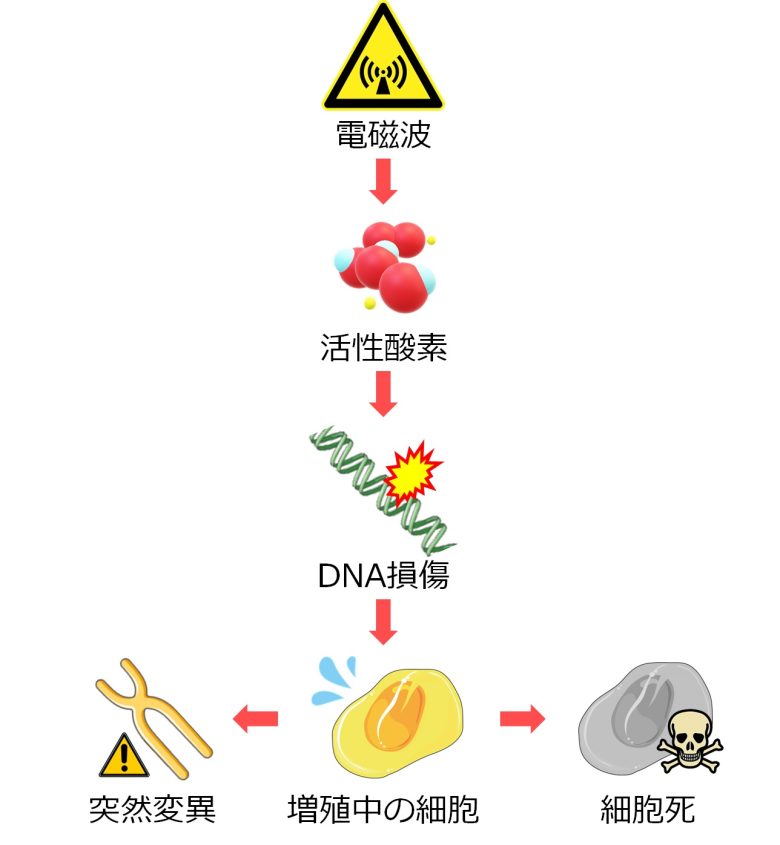
したがって細胞増殖が活発に行われている若い人ほど電磁波に脆弱であるということになり、これは上述の研究の観察結果と一致します。
電磁波がどのように細胞を損傷するのか、以下の記事で解説していますので、よろしければご覧ください。

前回の記事では、電磁波が健康に悪影響を及ぼすことを示した多数の研究を紹介しました。 この記事では続いて、その仕組みについて説明します。 電磁波は主として活性酸素を増加させることで、健康に悪影響を与える … 記事全文を読む
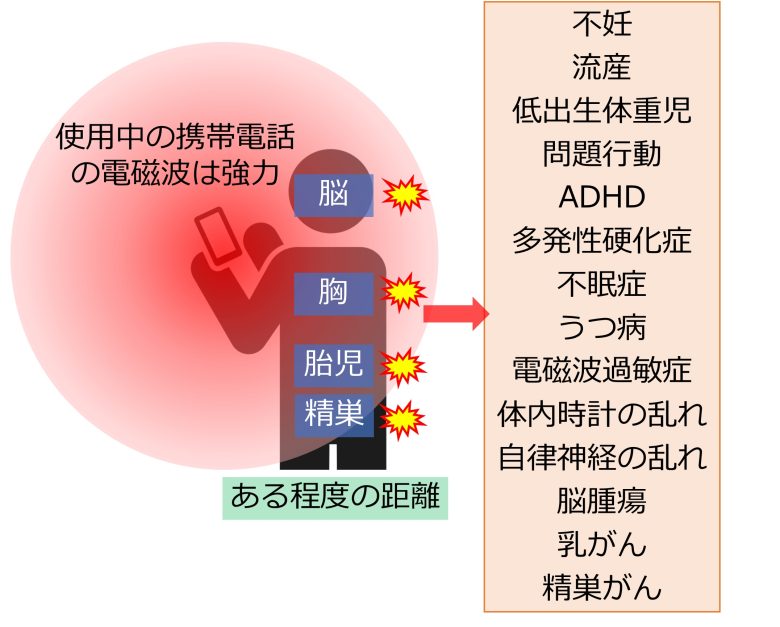
携帯電話の電磁波は危険
携帯電話の使用により、不妊 (精子減少)、流産、低出生体重児、問題行動、ADHD、多発性硬化症、不眠症、うつ病、電磁波過敏症、体内時計の乱れ (概日ホルモンの乱れ)、自律神経の乱れ、脳腫瘍、乳がん、精巣がんなどが増加しました。
これは、使用中の携帯電話の電磁波は強力で、使用時に近接する脳だけでなく、ある程度の距離にある胸や胎児、精巣にまでその悪影響を及ぼしていることを意味します。
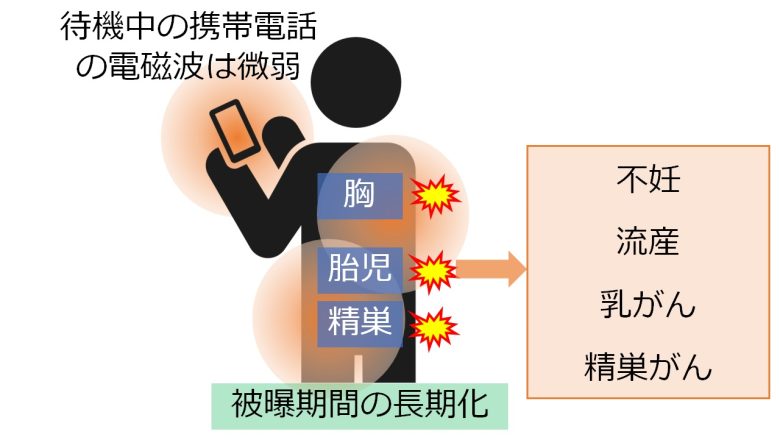
また、携帯電話の体近くの携帯によって不妊 (精子減少)、流産、乳がん、精巣がんなどが増加しました。
これは、待機中の携帯電話の電磁波は微弱ではあるものの、身体近くの所持により、胸や胎児、精巣での電磁波の被曝期間が長期化し、悪影響につながっていることを意味します。
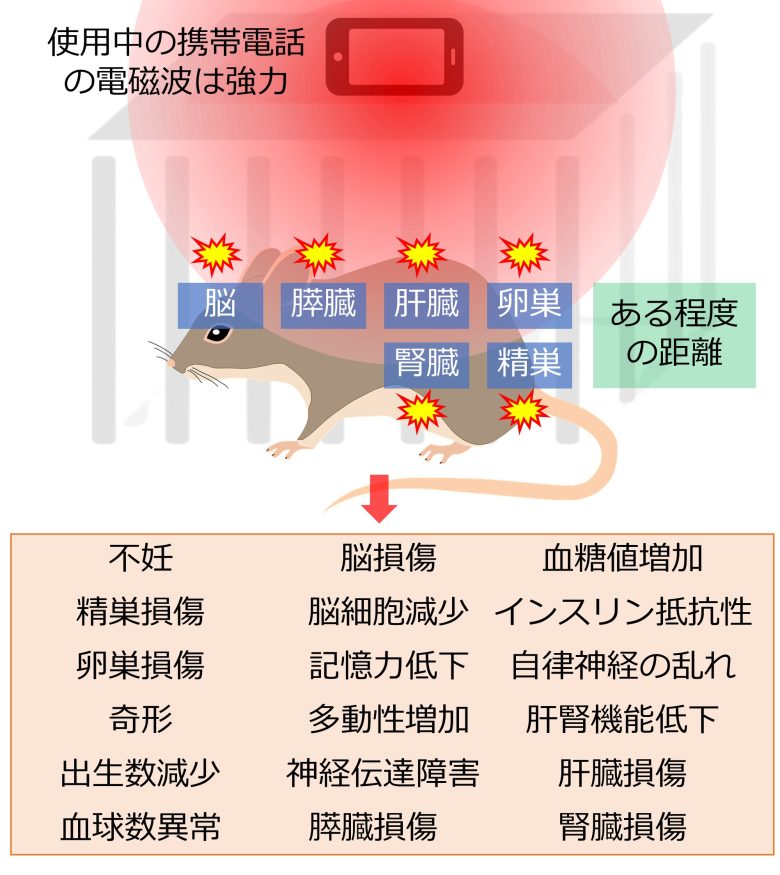
また動物実験でも、飼育ケージの上や床に携帯電話を設置すると、不妊 (精子減少、卵胞減少)、精巣損傷、卵巣損傷、奇形、出生数減少、血球数異常、脳損傷、脳細胞減少、記憶力低下、多動性増加、神経伝達障害、膵臓損傷、血糖値増加、インスリン抵抗性、自律神経の乱れ、肝機能低下、腎機能低下、肝臓損傷、腎臓損傷などが増加しました。
こちらも使用時の携帯電話の電磁波は強力で、ある程度離れた距離にいるマウスの脳や精巣や卵巣などに損傷を与えていることを意味します。
以上のように携帯電話の電磁波は強力で、生体に様々な影響をもたらします。
普及度から考えても、携帯電話が現在の人々の健康に及ぼしている影響は、非常に大きいものと考えられます。
妊娠中、未成年者、妊活中の携帯電話の利用は控える
先述の通り、若い人ほど電磁波に脆弱です。
つまり携帯電話の利用による不妊、脳細胞減少、記憶力低下、多動性増加、問題行動、がんなどの健康への影響を、より受けやすいといえます。
胎児においては、さらに流産や奇形、低出生体重のリスクもあります。
したがって妊娠中の女性や、未成年者の携帯電話の利用は極力控えるべきです。
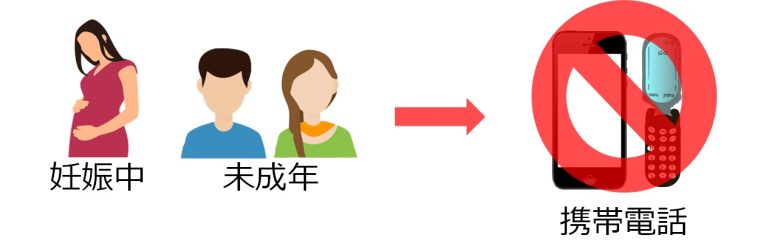
また、現在妊活中・予定のある方についても、携帯電話の利用により精巣・卵巣・受精卵 (胚) が損傷し、不妊になる恐れがあるため、その利用は極力控えるべきです。

携帯電話の代用品
デスクトップパソコンと液晶PCモニタ
携帯電話の機能のいくつかは、無線機能が無いかオフにしたデスクトップパソコンと、液晶PCモニタの組み合わせで代用できます。
双方とも高周波電磁波はほぼ放たず、極低周波の磁界はパソコンは30cmの距離で0 - 0.11μT、液晶PCモニタで0 μTと (The Electric Power Research Institute)、危険水準を双方ともほぼ下回っています。
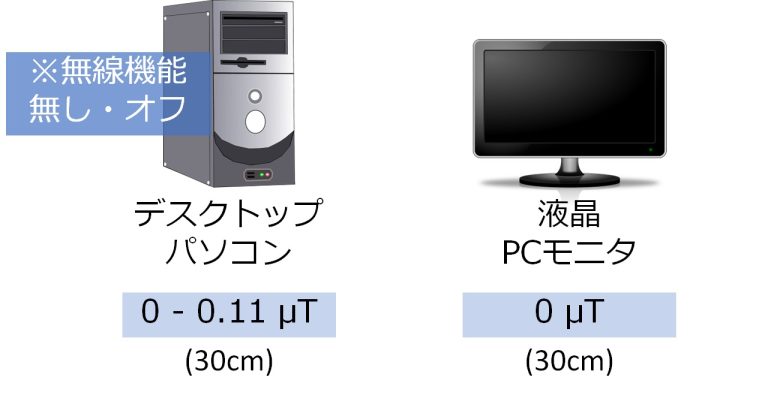
これらの製品は極低周波の電界は発しますが、前ページで説明した通り、電界は磁界に比べて、人体に大きな影響を与えるとは現在のところは考えられていません。
従って携帯電話に比べれば比較的安全に使用できると言えます。
インターネット通話、有線の固定電話
電話機能については、パソコンを経由したインターネット通話や、有線の固定電話などで代用するのが安全といえます。

コードレス電話は脳腫瘍をはじめとしたがんとの相関がいくつかの研究で確認されているため、お勧めできません。
電化製品の電磁波は危険
電化製品の使用により、不妊、流産、先天異常、体内時計の乱れ (概日ホルモンの乱れ)、自律神経の乱れ、がんが増加しました。

これらの製品はテレビやビデオ表示端末、電気毛布や電動ミシン、保育器などで、すべて数μTの電磁波を発します。
前ページでも触れましたが、一般的な電化製品は上記製品同様、数μT程度の低周波電磁波を発するものが多いです。
従って実際にリスク上昇が示された製品に限らず、電化製品への接近、特に長期間の接近は避けるべきです。
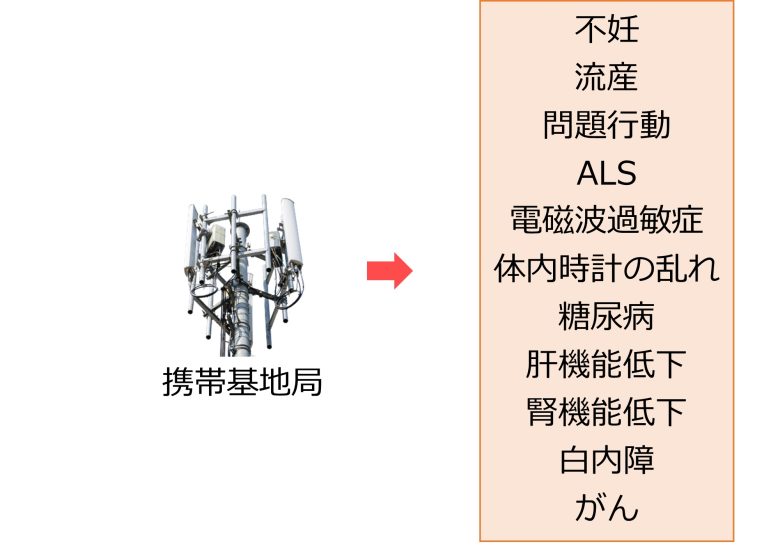
携帯基地局、高圧線、電波塔の電磁波は危険
携帯基地局の電磁波被曝で不妊、流産、問題行動、ALS、電磁波過敏症、体内時計の乱れ (概日ホルモンの乱れ)、糖尿病、肝機能低下、腎機能低下、白内障、がんが増加しました。
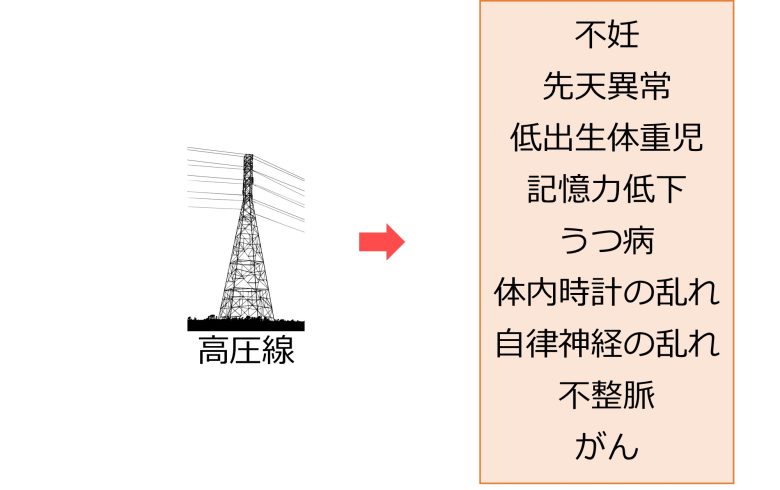
高圧線からの電磁波被曝で不妊、先天異常、低出生体重児、記憶力低下、うつ病、体内時計の乱れ (概日ホルモンの乱れ)、自律神経の乱れ、不整脈、がんが増加しました。
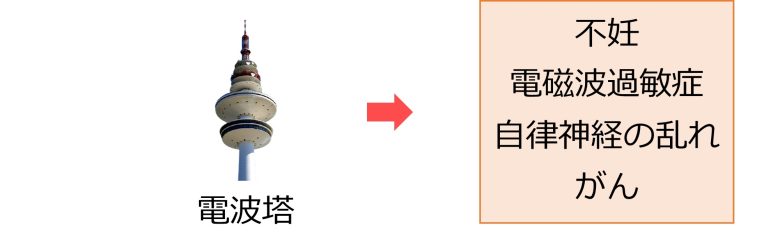
電波塔からの電磁波被曝で不妊、電磁波過敏症、自律神経の乱れ、がんが増加しました。
したがって高圧線、携帯基地局、電波塔からの電磁波被曝も極力避けるべきです。
携帯基地局、電波塔、高圧線の電磁波を防ぐには?
電磁シールドにより携帯基地局や電波塔などからの高周波電磁波を低減することは可能です。
たとえば2010年のオーストリアの研究では、電磁シールドの塗料 (YSHIELD®) を壁の1面残して全面に塗り、残り1面を電磁シールドのカーテン (Swiss Shield®) で覆うことで、携帯基地局の電磁波を強0.21 μW/cm2、中0.015 μW/cm2、弱0.00052 μW/cm2の3種類に調節しています。(Augner et al. 2010)
ただし、電磁波は障害物を回り込んで進む性質 (回折) があるため、壁やドア、窓などを対策しても、隙間があるとそこから入ってきてしまいます。
つまり個人で対策しても期待したほどの効果が得られない場合があることに注意すべきです。
対策にはお金や手間がかかるため、事前によく調べるか、あるいはプロに頼むのが良いと思われます。
なお、高圧線などの低周波電磁波 (極低周波の磁界) に関しては、電磁シールドでは遮蔽することができません。
食事で電磁波対策
電磁波による健康への影響は主として活性酸素の増加に起因しています。
そして、主に動物実験での確認とはなりますが、電磁波被曝と同時に抗酸化物質を摂取することで、その被害が軽減されることが示されています。
従って抗酸化作用のある食品や、抗酸化物質であるビタミンC、ビタミンE、ビタミンAを多く含む食品をとることで、電磁波による健康への影響を軽減できると考えられます。
ただしビタミンのサプリメントはお勧めできません。
なぜならサプリメントによる健康への悪影響というものが、いくつかの研究で示されているからです。
たとえば、ビタミンAの前駆体である、βカロチンを食事から摂取すると、肺がんのリスクが減少しましたが、サプリメントから摂取すると、逆に肺がんのリスクが上昇しました。(Albanes 1999)
また、ビタミンCとEのサプリメントの妊娠期間中の服用で低出生体重児が増加し(Poston et al. 2006)、ビタミンEのサプリメントの服用で前立腺がんのリスクが上昇しました。(Klein et al. 2011)
さらなる証拠が見たい方へ
この記事では200件の電磁波の健康影響を示す研究を紹介しました。
もっと証拠が見たいという方には、2022年に更新されたバイオイニシャティブ2012の報告がおすすめです。この報告によれば、遺伝子、神経学、酸化損傷に関する2206件の研究のうち、1779件もが電磁波による生体効果を認めています。(Bioinitiative 2022)
この他にもストレス反応、免疫反応、小児がん、脳腫瘍、乳がん、生殖機能、胎児や新生児、自閉症などに関して、非常に多数の研究が網羅されています。(Bioinitiative 2022)
また、環境への影響も指摘されています (Environmental Health Trust)。Levittらは、1200以上の科学的文献を引用した、野生生物への悪影響に関する3部構成の画期的な研究レビューを2021年に発表しました (Levitt et al. 2021, Levitt et al. 2021, Levitt et al. 2021)。
画像の帰属
この記事における以下の画像はServier Medical Artに帰属します。
精巣、精子、卵巣、卵胞、胎児、マウス、マウスの胎児、ホルモン、人体のシルエット、視交叉上核、下垂体、副腎、ニューロンと髄鞘、神経接続部、肺、血管、ブドウ糖、膵臓、インスリン、筋肉、脂肪細胞、受容体、輸送体、自律神経、瞳、唾液腺、胃、膀胱、肝臓、腎臓、眼球、水晶体、腫瘍、骨、リンパ節、造血幹細胞、骨髄系細胞、リンパ系細胞、髄膜、内耳神経、乳房、皮膚、前立腺、DNA二重鎖、細胞、染色体、DNA付き細胞。
ServierのServier Medical Artは、Creative Commons Attribution 3.0 Unported Licenseの規定に従い使用を許諾されます。
参考文献
1. Sengupta P. 2013. The Laboratory Rat: Relating Its Age With Human’s. International journal of preventive medicine. 4(6):624–30. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/23930179/.
2. Dutta S, Sengupta P. 2016. Men and mice: Relating their ages. Life Sciences. 152:244–248. doi:10.1016/j.lfs.2015.10.025. http://dx.doi.org/10.1016/j.lfs.2015.10.025.
3. Amrhein V, Greenland S, McShane B. 2019. Scientists rise up against statistical significance. Nature. 567(7748):305–307. doi:10.1038/d41586-019-00857-9. http://dx.doi.org/10.1038/d41586-019-00857-9.
4. Fyodorov DV, Zhou B-R, Skoultchi AI, Bai Y. 2017. Emerging roles of linker histones in regulating chromatin structure and function. Nature Reviews Molecular Cell Biology. 19(3):192–206. doi:10.1038/nrm.2017.94. http://dx.doi.org/10.1038/nrm.2017.94.
5. Gyori BM, Venkatachalam G, Thiagarajan PS, Hsu D, Clement M-V. 2014. OpenComet: An automated tool for comet assay image analysis. Redox Biology. 2:457–465. doi:10.1016/j.redox.2013.12.020. http://dx.doi.org/10.1016/j.redox.2013.12.020.
6. Institute of Electrical and Electronics Engineers. Biological and health effects of electric and magnetic fields from video display terminals. [accessed 2023 Jul 6]. https://ieeexplore.ieee.org/document/585523.
7. The Electric Power Research Institute. Magnetic Fields from Electrical Appliances and Devices. [accessed 2023 Jul 18]. http://www.epri.com/research/products/000000000001021221.
8. Akakin D, Tok OE, Anil D, Akakin A, Sirvanci S, Sener G, Ercan F. 2020. Electromagnetic waves from mobile phones may affect rat brain during development. Turkish Neurosurgery. doi:10.5137/1019-5149.jtn.31665-20.2. http://dx.doi.org/10.5137/1019-5149.jtn.31665-20.2.
9. Hasan I, Amin T, Alam MR, Islam MR. 2021. Hematobiochemical and histopathological alterations of kidney and testis due to exposure of 4G cell phone radiation in mice. Saudi Journal of Biological Sciences. 28(5):2933–2942. doi:10.1016/j.sjbs.2021.02.028. http://dx.doi.org/10.1016/j.sjbs.2021.02.028.
10. Delgado JM, Leal J, Monteagudo JL, Gracia MG. 1982. Embryological changes induced by weak, extremely low frequency electromagnetic fields. Journal of anatomy. 134(Pt 3):533–51. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/7107514/.
11. Mortazavi SMJ, Owji SM, Shojaei-Fard MB, Ghader-Panah M, Mortazavi SAR, Tavakoli-Golpayegani A, Haghani M, Taeb S, Shokrpour N, Koohi O. 2016. GSM 900 MHz Microwave Radiation-Induced Alterations of Insulin Level and Histopathological Changes of Liver and Pancreas in Rat. Journal of biomedical physics & engineering. 6(4):235–242. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/28144593/.
12. Programme for International Student Assessment. PISA. [accessed 2023 Jun 21]. https://www.oecd.org/pisa/.
13. Weintraub K. 2011. The prevalence puzzle: Autism counts. Nature. 479(7371):22–24. doi:10.1038/479022a. http://dx.doi.org/10.1038/479022a.
14. CDC NHIS. National Health Interview Survey 1997-2018. [accessed 2023 Nov 19]. https://www.cdc.gov/nchs/nhis/1997-2018.htm.
15. Ministry of Education, Culture, Sports, Science and Technology. Heisei 28 Nendo Tuukyuu Niyoru Sidou Jisshi Joukyou Kekka ni Tuite (Results of the Survey on the Status of Implementation of Guidance through Classroom Instruction in Fiscal Year 2008). [accessed 2023 Jun 21]. https://www.mext.go.jp/a_menu/shotou/tokubetu/material/1383567.htm.
16. CDC WONDER. National Center for Health Statistics Mortality Data on CDC WONDER. [accessed 2023 Nov 18]. https://wonder.cdc.gov/Deaths-by-Underlying-Cause.html.
17. Statistics Finland. Deaths from dementia and Alzheimer’s disease in 1969 to 2010. [accessed 2023 Jun 21]. https://www.stat.fi/til/ksyyt/2010/ksyyt_2010_2011-12-16_kat_003_en.html.
18. Statistics of Japan. Vital Statistics. [accessed 2023 Nov 19]. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450011&tstat=000001028897.
19. Hallberg Ö. 2015. Alzheimer mortality - why does it increase so fast in sparsely populated areas? Bioelectromagnetics. 1(1):225–246. https://www.researchgate.net/publication/262168098.
20. Fang F, Valdimarsdóttir U, Bellocco R, Ronnevi L-O, Sparén P, Fall K, Ye W. 2009. Amyotrophic Lateral Sclerosis in Sweden, 1991-2005. Archives of Neurology. 66(4). doi:10.1001/archneurol.2009.13. http://dx.doi.org/10.1001/archneurol.2009.13.
21. Japan Intractable Diseases Information Center. Tokutei Shikkan Iryou Jukyuusya-Shou Syojisya-Suu (Number of holders of medical care beneficiary certificates for specified diseases). [accessed 2023 Jun 21]. https://www.nanbyou.or.jp/entry/1356.
22. Alonso A, Hernán MA. 2008. Temporal trends in the incidence of multiple sclerosis. Neurology. 71(2):129–135. doi:10.1212/01.wnl.0000316802.35974.34. http://dx.doi.org/10.1212/01.wnl.0000316802.35974.34.
23. Weinberger AH, Gbedemah M, Martinez AM, Nash D, Galea S, Goodwin RD. 2017. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychological Medicine. 48(8):1308–1315. doi:10.1017/s0033291717002781. http://dx.doi.org/10.1017/s0033291717002781.
24. Ministry of Health, Labour and Welfare. Kongo no Seishin Hoken Iryou Hukushi no Arikata Nado ni Kansuru Kentou-kai (Dai 18 Kai) (Study Group on Future Mental Health and Medical Welfare (18th meeting)). [accessed 2023 Jun 21]. https://www.mhlw.go.jp/shingi/2009/06/s0604-7.html.
25. Statistics of Japan. Patient Survey. [accessed 2023 Nov 20]. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450022&tstat=000001031167.
26. CDC WISQARS. Injury Prevention & Control. [accessed 2023 Nov 13]. https://www.cdc.gov/injury/wisqars/index.html.
27. Thomas S, Heinrich S, von Kries R, Radon K. 2009. Exposure to radio-frequency electromagnetic fields and behavioural problems in Bavarian children and adolescents. European Journal of Epidemiology. 25(2):135–141. doi:10.1007/s10654-009-9408-x. http://dx.doi.org/10.1007/s10654-009-9408-x.
28. Divan HA, Kheifets L, Obel C, Olsen J. 2008. Prenatal and Postnatal Exposure to Cell Phone Use and Behavioral Problems in Children. Epidemiology. 19(4):523–529. doi:10.1097/ede.0b013e318175dd47. http://dx.doi.org/10.1097/ede.0b013e318175dd47.
29. Guxens M, van Eijsden M, Vermeulen R, Loomans E, Vrijkotte TGM, Komhout H, van Strien RT, Huss A. 2013. Maternal cell phone and cordless phone use during pregnancy and behaviour problems in 5-year-old children. Journal of Epidemiology and Community Health. 67(5):432–438. doi:10.1136/jech-2012-201792. http://dx.doi.org/10.1136/jech-2012-201792.
30. Byun Y-H, Ha M, Kwon H-J, Hong Y-C, Leem J-H, Sakong J, Kim SY, Lee CG, Kang D, Choi H-D, et al. 2013. Mobile Phone Use, Blood Lead Levels, and Attention Deficit Hyperactivity Symptoms in Children: A Longitudinal Study. Scott JG, editor. PLoS ONE. 8(3):e59742. doi:10.1371/journal.pone.0059742. http://dx.doi.org/10.1371/journal.pone.0059742.
31. Ghadamgahi M, Monazzam MR, Hosseini M. 2016. Memory loss risk assessment for the students nearby high-voltage power lines—a case study. Environmental Monitoring and Assessment. 188(6). doi:10.1007/s10661-016-5358-4. http://dx.doi.org/10.1007/s10661-016-5358-4.
32. Feychting M, Pedersen N, Svedberg P, Floderus B, Gatz M. 1998. Dementia and occupational exposure to magnetic fields. Scandinavian Journal of Work, Environment & Health. 24(1):46–53. doi:10.5271/sjweh.277. http://dx.doi.org/10.5271/sjweh.277.
33. Sobel E, Davanipour Z, Sulkava R, Erkinjuntti T, Wikstrom J, Henderson VW, Buckwalter G, Bowman JD, Lee P-J. 1995. Occupations with Exposure to Electromagnetic Fields: A Possible Risk Factor for Alzheimer’s Disease. American Journal of Epidemiology. 142(5):515–524. doi:10.1093/oxfordjournals.aje.a117669. http://dx.doi.org/10.1093/oxfordjournals.aje.a117669.
34. Håkansson N, Gustavsson P, Johansen C, Floderus B. 2003. Neurodegenerative Diseases in Welders and Other Workers Exposed to High Levels of Magnetic Fields. Epidemiology. 14(4):420–426. doi:10.1097/01.ede.0000078446.76859.c9. http://dx.doi.org/10.1097/01.ede.0000078446.76859.c9.
35. Luna J, Leleu J-P, Preux P-M, Corcia P, Couratier Philippe, Marin Benoit, Boumediene F, Marin B., Couratier P., Preux PM, et al. 2019. Residential exposure to ultra high frequency electromagnetic fields emitted by Global System for Mobile (GSM) antennas and amyotrophic lateral sclerosis incidence: A geo-epidemiological population-based study. Environmental Research. 176:108525. doi:10.1016/j.envres.2019.108525. http://dx.doi.org/10.1016/j.envres.2019.108525.
36. Harbo Poulsen A, Stenager E, Johansen C, Bentzen J, Friis S, Schüz J. 2012. Mobile Phones and Multiple Sclerosis – A Nationwide Cohort Study in Denmark. Kira J, editor. PLoS ONE. 7(4):e34453. doi:10.1371/journal.pone.0034453. http://dx.doi.org/10.1371/journal.pone.0034453.
37. Savitz DA, Checkoway H, Loomis DP. 1998. Magnetic field exposure and neurodegenerative disease mortality among electric utility workers. Epidemiology (Cambridge, Mass). 9(4):398–404. [accessed 2024 Mar 17]. https://pubmed.ncbi.nlm.nih.gov/9647903/.
38. Harmanci H, Emre M, Gurvit H, Bilgic B, Hanagasi H, Gurol E, Sahin H, Tinaz S. 2003. Risk Factors for Alzheimer Disease: A Population-Based Case-Control Study in Istanbul, Turkey. Alzheimer Disease & Associated Disorders. 17(3):139–145. doi:10.1097/00002093-200307000-00003. http://dx.doi.org/10.1097/00002093-200307000-00003.
39. Johansen C. 2000. Exposure to Electromagnetic Fields and Risk of Central Nervous System Disease in Utility Workers. Epidemiology. 11(5):539–543. doi:10.1097/00001648-200009000-00009. http://dx.doi.org/10.1097/00001648-200009000-00009.
40. JORTNER B. 2006. The return of the dark neuron. A histological artifact complicating contemporary neurotoxicologic evaluation. NeuroToxicology. 27(4):628–634. doi:10.1016/j.neuro.2006.03.002. http://dx.doi.org/10.1016/j.neuro.2006.03.002.
41. Nilufer Yonguc G, Dodurga Y, Kurtulus A, Boz B, Acar K. 2012. Caspase 1, Caspase 3, TNF-alpha, p53, and Hif1-alpha gene expression status of the brain tissues and hippocampal neuron loss in short-term dichlorvos exposed rats. Molecular Biology Reports. 39(12):10355–10360. doi:10.1007/s11033-012-1913-4. http://dx.doi.org/10.1007/s11033-012-1913-4.
42. Dhikav V, Anand K. 2011. Potential Predictors of Hippocampal Atrophy in Alzheimerʼs Disease. Drugs & Aging. 28(1):1–11. doi:10.2165/11586390-000000000-00000. http://dx.doi.org/10.2165/11586390-000000000-00000.
43. Hoogman M, Bralten J, Hibar DP, Mennes M, Zwiers MP, Schweren LSJ, van Hulzen KJE, Medland SE, Shumskaya E, Jahanshad N, et al. 2017. Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis. The Lancet Psychiatry. 4(4):310–319. doi:10.1016/s2215-0366(17)30049-4. http://dx.doi.org/10.1016/s2215-0366(17)30049-4.
44. Videbech P. 2004. Hippocampal Volume and Depression: A Meta-Analysis of MRI Studies. American Journal of Psychiatry. 161(11):1957–1966. doi:10.1176/appi.ajp.161.11.1957. http://dx.doi.org/10.1176/appi.ajp.161.11.1957.
45. Deweer B, Lehericy S, Pillon B, Baulac M, Chiras J, Marsault C, Agid Y, Dubois B. 1995. Memory disorders in probable Alzheimer’s disease: the role of hippocampal atrophy as shown with MRI. Journal of Neurology, Neurosurgery & Psychiatry. 58(5):590–597. doi:10.1136/jnnp.58.5.590. http://dx.doi.org/10.1136/jnnp.58.5.590.
46. Isaacs EB, Lucas A, Chong WK, Wood SJ, Johnson CL, Marshall C, Vargha-Khadem F, Gadian DG. 2000. Hippocampal Volume and Everyday Memory in Children of Very Low Birth Weight. Pediatric Research. 47(6):713–720. doi:10.1203/00006450-200006000-00006. http://dx.doi.org/10.1203/00006450-200006000-00006.
47. Aanes S, Bjuland KJ, Sripada K, Sølsnes AE, Grunewaldt KH, Håberg A, Løhaugen GC, Skranes J. 2019. Reduced hippocampal subfield volumes and memory function in school-aged children born preterm with very low birthweight (VLBW). NeuroImage: Clinical. 23:101857. doi:10.1016/j.nicl.2019.101857. http://dx.doi.org/10.1016/j.nicl.2019.101857.
48. Sheline YI, Sanghavi M, Mintun MA, Gado MH. 1999. Depression Duration But Not Age Predicts Hippocampal Volume Loss in Medically Healthy Women with Recurrent Major Depression. The Journal of Neuroscience. 19(12):5034–5043. doi:10.1523/jneurosci.19-12-05034.1999. http://dx.doi.org/10.1523/jneurosci.19-12-05034.1999.
49. Gupta P, Soyombo AA, Atashband A, Wisniewski KE, Shelton JM, Richardson JA, Hammer RE, Hofmann SL. 2001. Disruption ofPPT1orPPT2causes neuronal ceroid lipofuscinosis in knockout mice. Proceedings of the National Academy of Sciences. 98(24):13566–13571. doi:10.1073/pnas.251485198. http://dx.doi.org/10.1073/pnas.251485198.
50. Kinnear Kern J. 2003. Purkinje cell vulnerability and autism: a possible etiological connection. Brain and Development. 25(6):377–382. doi:10.1016/s0387-7604(03)00056-1. http://dx.doi.org/10.1016/s0387-7604(03)00056-1.
51. Salford LG, Brun AE, Eberhardt JL, Malmgren L, Persson BRR. 2003. Nerve cell damage in mammalian brain after exposure to microwaves from GSM mobile phones. Environmental Health Perspectives. 111(7):881–883. doi:10.1289/ehp.6039. http://dx.doi.org/10.1289/ehp.6039.
52. Odaci E, Bas O, Kaplan S. 2008. Effects of prenatal exposure to a 900 MHz electromagnetic field on the dentate gyrus of rats: a stereological and histopathological study. Brain Research. 1238:224–229. doi:10.1016/j.brainres.2008.08.013. http://dx.doi.org/10.1016/j.brainres.2008.08.013.
53. Bas O, Odaci E, Mollaoglu H, Ucok K, Kaplan S. 2009. Chronic prenatal exposure to the 900 megahertz electromagnetic field induces pyramidal cell loss in the hippocampus of newborn rats. Toxicology and Industrial Health. 25(6):377–384. doi:10.1177/0748233709106442. http://dx.doi.org/10.1177/0748233709106442.
54. Kim JH, Yu D-H, Huh YH, Lee EH, Kim H-G, Kim HR. 2017. Long-term exposure to 835 MHz RF-EMF induces hyperactivity, autophagy and demyelination in the cortical neurons of mice. Scientific Reports. 7(1). doi:10.1038/srep41129. http://dx.doi.org/10.1038/srep41129.
55. Sonmez OF, Odaci E, Bas O, Kaplan S. 2010. Purkinje cell number decreases in the adult female rat cerebellum following exposure to 900MHz electromagnetic field. Brain Research. 1356:95–101. doi:10.1016/j.brainres.2010.07.103. http://dx.doi.org/10.1016/j.brainres.2010.07.103.
56. Ali M, Shah MAA, Aftab MI, Mushtaq F, Mehmood F, Mobushir M, Ali BA. 2020. Effect of Electromagnetic Field (EMF) of cellular phones on purkinje cell margins and perineuronal space in the cortex of rat cerebellum. Pakistan Journal of Medical and Health. 14(4):958–961. https://www.researchgate.net/publication/355719951.
57. Megha K, Deshmukh PS, Banerjee BD, Tripathi AK, Ahmed R, Abegaonkar MP. 2015. Low intensity microwave radiation induced oxidative stress, inflammatory response and DNA damage in rat brain. NeuroToxicology. 51:158–165. doi:10.1016/j.neuro.2015.10.009. http://dx.doi.org/10.1016/j.neuro.2015.10.009.
58. Afeefy AA, Afifi OK, Tolba AMA. 2013. A Histological and Immunohistochemical study on the effect of mobile phone radiation on the hipocampus of adult and newborn albino rats. Nature and Science. 11(8):98–113. https://www.researchgate.net/publication/320922211_A_Histological_and_Immunohistochemical_study_on_the_effect_of_mobile_phone_radiation_on_the_hipocampus_of_adult_and_newborn_albino_rats.
59. Bas O, Odaci E, Kaplan S, Acer N, Ucok K, Colakoglu S. 2009. 900 MHz electromagnetic field exposure affects qualitative and quantitative features of hippocampal pyramidal cells in the adult female rat. Brain Research. 1265:178–185. doi:10.1016/j.brainres.2009.02.011. http://dx.doi.org/10.1016/j.brainres.2009.02.011.
60. Bas O, Sonmez OF, Aslan A, Keleş Aİ. 2013. Pyramidal Cell Loss in the Cornu Ammonis of 32-day-old Female Rats Following Exposure to a 900 Megahertz Electromagnetic Field During Prenatal Days 13-21. NeuroQuantology. 11(4):591–599. https://www.researchgate.net/publication/264913627/.
61. Rağbetlı MC, Aydinlioğlu A, Koyun N, Rağbetlı C, Bektas Ş, Ozdemır S. 2010. The effect of mobile phone on the number of Purkinje cells: A stereological study. International Journal of Radiation Biology. 86(7):548–554. doi:10.3109/09553001003734527. http://dx.doi.org/10.3109/09553001003734527.
62. Herbert MR, Sage C. 2013. Autism and EMF? Plausibility of a pathophysiological link – Part I. Pathophysiology. 20(3):191–209. doi:10.1016/j.pathophys.2013.08.001. http://dx.doi.org/10.1016/j.pathophys.2013.08.001.
63. İkinci A, Odaci E, Yildirim M, Kaya H, Akça M, Hancı H, Asşan A, Sönmez OF, Baş O. 2013. The effects of prenatal exposure to a 900 megahertz electromagnetic field on hippocampus morphology and learning behavior in rat pups. Journal of Experimental & Clinical Medicine. 30(3):278. https://www.researchgate.net/publication/315135914/.
64. Narayanan SN, Kumar RS, Potu BK, Nayak S, Mailankot M. 2009. Spatial Memory Perfomance of Wistar Rats Exposed to Mobile Phone. Clinics. 64(3):231–234. doi:10.1590/s1807-59322009000300014. http://dx.doi.org/10.1590/s1807-59322009000300014.
65. Narayanan SN, Kumar RS, Potu BK, Nayak S, Bhat PG, Mailankot M. 2010. Effect of radio-frequency electromagnetic radiations (RF-EMR) on passive avoidance behaviour and hippocampal morphology in Wistar rats. Upsala Journal of Medical Sciences. 115(2):91–96. doi:10.3109/03009730903552661. http://dx.doi.org/10.3109/03009730903552661.
66. Gao Q-H, Cai Q, Fan Y. 2017. Beneficial effect of catechin and epicatechin on cognitive impairment and oxidative stress induced by extremely low frequency electromagnetic field. Journal of Food Biochemistry. 41(6):e12416. doi:10.1111/jfbc.12416. http://dx.doi.org/10.1111/jfbc.12416.
67. Nittby H, Grafström G, Tian DP, Malmgren L, Brun A, Persson BRR, Salford LG, Eberhardt J. 2007. Cognitive impairment in rats after long‐term exposure to GSM‐900 mobile phone radiation. Bioelectromagnetics. 29(3):219–232. doi:10.1002/bem.20386. http://dx.doi.org/10.1002/bem.20386.
68. Maaroufi K, Had-Aissouni L, Melon C, Sakly M, Abdelmelek H, Poucet B, Save E. 2014. Spatial learning, monoamines and oxidative stress in rats exposed to 900MHz electromagnetic field in combination with iron overload. Behavioural Brain Research. 258:80–89. doi:10.1016/j.bbr.2013.10.016. http://dx.doi.org/10.1016/j.bbr.2013.10.016.
69. Save E, Poucet B, Foreman N, Buhot MC. 1992. Object exploration and reactions to spatial and nonspatial changes in hooded rats following damage to parietal cortex or hippocampal formation. Behavioral neuroscience. 106(3):447–56. [accessed 2024 Mar 17]. https://pubmed.ncbi.nlm.nih.gov/1616611/.
70. Lee I, Hunsaker MR, Kesner RP. 2005. The Role of Hippocampal Subregions in Detecting Spatial Novelty. Behavioral Neuroscience. 119(1):145–153. doi:10.1037/0735-7044.119.1.145. http://dx.doi.org/10.1037/0735-7044.119.1.145.
71. Aldad TS, Gan G, Gao X-B, Taylor HS. 2012. Fetal Radiofrequency Radiation Exposure From 800-1900 Mhz-Rated Cellular Telephones Affects Neurodevelopment and Behavior in Mice. Scientific Reports. 2(1). doi:10.1038/srep00312. http://dx.doi.org/10.1038/srep00312.
72. Verkasalo p. K, Kaprio J, Varjonen J, Romanov K, Heikkila K, Koskenvuo M. 1997. Magnetic Fields of Transmission Lines and Depression. American Journal of Epidemiology. 146(12):1037–1045. doi:10.1093/oxfordjournals.aje.a009232. http://dx.doi.org/10.1093/oxfordjournals.aje.a009232.
73. Tamura H, Nishida T, Tsuji A, Sakakibara H. 2017. Association between Excessive Use of Mobile Phone and Insomnia and Depression among Japanese Adolescents. International Journal of Environmental Research and Public Health. 14(7):701. doi:10.3390/ijerph14070701. http://dx.doi.org/10.3390/ijerph14070701.
74. van Wijngaarden E. 2000. Exposure to electromagnetic fields and suicide among electric utility workers: a nested case-control study. Occupational and Environmental Medicine. 57(4):258–263. doi:10.1136/oem.57.4.258. http://dx.doi.org/10.1136/oem.57.4.258.
75. Baris D, Armstrong B. 1990. Suicide among electric utility workers in England and Wales. Occupational and Environmental Medicine. 47(11):788–789. doi:10.1136/oem.47.11.788. http://dx.doi.org/10.1136/oem.47.11.788.
76. Perry SF, Reichmanis M, Marino AA, Becker RO. 1981. Environmental Power-frequency Magnetic Fields and Suicide. Health Physics. 41(2):267–277. doi:10.1097/00004032-198108000-00003. http://dx.doi.org/10.1097/00004032-198108000-00003.
77. van Wijngaarden E. 2003. An Exploratory Investigation of Suicide and Occupational Exposure. Journal of Occupational and Environmental Medicine. 45(1):96–101. doi:10.1097/00043764-200301000-00018. http://dx.doi.org/10.1097/00043764-200301000-00018.
78. Carpenter DO. 2015. The microwave syndrome or electro-hypersensitivity: historical background. Reviews on Environmental Health. 30(4). doi:10.1515/reveh-2015-0016. http://dx.doi.org/10.1515/reveh-2015-0016.
79. Stein Y, Udasin IG. 2020. Electromagnetic hypersensitivity (EHS, microwave syndrome) – Review of mechanisms. Environmental Research. 186:109445. doi:10.1016/j.envres.2020.109445. http://dx.doi.org/10.1016/j.envres.2020.109445.
80. Santini R, Santini P, Danze JM, Le Ruz P, Seigne M. 2002. Enquête sur la santé de riverains de stations relais de téléphonie mobile : I/Incidences de la distance et du sexe. Pathologie Biologie. 50(6):369–373. doi:10.1016/s0369-8114(02)00311-5. http://dx.doi.org/10.1016/s0369-8114(02)00311-5.
81. Abelin T, Altpeter E, Roosli M. 2005. Sleep Disturbances in the Vicinity of the Short-Wave Broadcast Transmitter Schwarzenburg. Schlafstorungen in der Umgebung des Kurzwellensenders Schwarzenburg. Somnologie. 9(4):203–209. doi:10.1111/j.1439-054x.2005.00072.x. http://dx.doi.org/10.1111/j.1439-054x.2005.00072.x.
82. Preece AW, Georgiou AG, Dunn EJ, Farrow SC. 2006. Health response of two communities to military antennae in Cyprus. Occupational and Environmental Medicine. 64(6):402–408. doi:10.1136/oem.2006.028894. http://dx.doi.org/10.1136/oem.2006.028894.
83. Sandstrom M. 2001. Mobile phone use and subjective symptoms. Comparison of symptoms experienced by users of analogue and digital mobile phones. Occupational Medicine. 51(1):25–35. doi:10.1093/occmed/51.1.25. http://dx.doi.org/10.1093/occmed/51.1.25.
84. Hutter H-P. 2006. Subjective symptoms, sleeping problems, and cognitive performance in subjects living near mobile phone base stations. Occupational and Environmental Medicine. 63(5):307–313. doi:10.1136/oem.2005.020784. http://dx.doi.org/10.1136/oem.2005.020784.
85. Söderqvist F, Carlberg M, Hardell L. 2008. Use of wireless telephones and self-reported health symptoms: a population-based study among Swedish adolescents aged 15–19 years. Environmental Health. 7(1). doi:10.1186/1476-069x-7-18. http://dx.doi.org/10.1186/1476-069x-7-18.
86. Menaker M, Murphy ZC, Sellix MT. 2013. Central control of peripheral circadian oscillators. Current Opinion in Neurobiology. 23(5):741–746. doi:10.1016/j.conb.2013.03.003. http://dx.doi.org/10.1016/j.conb.2013.03.003.
87. Jarupat S, Kawabata A, Tokura H, Borkiewicz A. 2003. Effects of the 1900MHz Electromagnetic Field Emitted from Cellular Phone on Nocturnal Melatonin Secretion. Journal of PHYSIOLOGICAL ANTHROPOLOGY and Applied Human Science. 22(1):61–63. doi:10.2114/jpa.22.61. http://dx.doi.org/10.2114/jpa.22.61.
88. Burch JB, Reif JS, Noonan CW, Yost MG. 2000. Melatonin Metabolite Levels in Workers Exposed to 60-Hz Magnetic Fields: Journal of Occupational and Environmental Medicine. 42(2):136–142. doi:10.1097/00043764-200002000-00006. http://dx.doi.org/10.1097/00043764-200002000-00006.
89. Yellon SM. 1994. Acute 60 Hz magnetic field exposure effects on the melatonin rhythm in the pineal gland and circulation of the adult Djungarian hamster. Journal of Pineal Research. 16(3):136–144. doi:10.1111/j.1600-079x.1994.tb00093.x. http://dx.doi.org/10.1111/j.1600-079x.1994.tb00093.x.
90. Wilson BW, Anderson LE, Ian Hilton D, Phillips RD. 1981. Chronic exposure to 60‐Hz electric fields: Effects on pineal function in the rat. Bioelectromagnetics. 2(4):371–380. doi:10.1002/bem.2250020408. http://dx.doi.org/10.1002/bem.2250020408.
91. Augner C, Hacker GW, Oberfeld G, Florian M, Hitzl W, Hutter J, Pauser G. 2010. Effects of Exposure to GSM Mobile Phone Base Station Signals on Salivary Cortisol, Alpha-Amylase, and Immunoglobulin A. Biomedical and Environmental Sciences. 23(3):199–207. doi:10.1016/s0895-3988(10)60053-0. http://dx.doi.org/10.1016/s0895-3988(10)60053-0.
92. Mortazavi SMJ, Vazife-Doost S, Yaghooti M, Mehdizadeh S, Rajaie-Far A. 2012. Occupational exposure of dentists to electromagnetic fields produced by magnetostrictive cavitrons alters the serum cortisol level. Journal of natural science, biology, and medicine. 3(1):60–4. doi:10.4103/0976-9668.95958. [accessed 2024 Mar 17]. https://pubmed.ncbi.nlm.nih.gov/22690053/.
93. Juutilainen J, Stevens RG, Anderson LE, Hansen NH, Kilpeläinen M, Kumlin T, Laitinen JT, Sobel E, Wilson BW. 2000. Nocturnal 6‐hydroxymelatonin sulfate excretion in female workers exposed to magnetic fields. Journal of Pineal Research. 28(2):97–104. doi:10.1034/j.1600-079x.2001.280205.x. http://dx.doi.org/10.1034/j.1600-079x.2001.280205.x.
94. Mostafa RM, Mostafa YM, Ennaceur A. 2002. Effects of exposure to extremely low-frequency magnetic field of 2 G intensity on memory and corticosterone level in rats. Physiology & Behavior. 76(4–5):589–595. doi:10.1016/s0031-9384(02)00730-8. http://dx.doi.org/10.1016/s0031-9384(02)00730-8.
95. Bonhomme-Faivre L, Macé A, Bezie Y, Marion S, Bindoula G, Szekely AM, Frénois N, Auclair H, Orbach-Arbouys S, Bizi E. 1998. Alterations of biological parameters in mice chronically exposed to low-frequency (50 HZ) electromagnetic fields. Life Sciences. 62(14):1271–1280. doi:10.1016/s0024-3205(98)00057-5. http://dx.doi.org/10.1016/s0024-3205(98)00057-5.
96. Hiwaki O. Influence of 50 Hz magnetic fields on circadian rhythm of the suprachiasmatic nucleus activity. Proceedings of the 20th Annual International Conference of the IEEE Engineering in Medicine and Biology Society Vol20 Biomedical Engineering Towards the Year 2000 and Beyond (Cat No98CH36286). doi:10.1109/iembs.1998.746203. http://dx.doi.org/10.1109/iembs.1998.746203.
97. Thöni V, Oliva R, Mauracher D, Egg M. 2021. Therapeutic Nuclear Magnetic Resonance affects the core clock mechanism and associated Hypoxia-inducible factor-1. Chronobiology International. 38(8):1120–1134. doi:10.1080/07420528.2021.1910288. http://dx.doi.org/10.1080/07420528.2021.1910288.
98. Riemann D, Klein T, Rodenbeck A, Feige B, Horny A, Hummel R, Weske G, Al-Shajlawi A, Voderholzer U. 2002. Nocturnal cortisol and melatonin secretion in primary insomnia. Psychiatry Research. 113(1–2):17–27. doi:10.1016/s0165-1781(02)00249-4. http://dx.doi.org/10.1016/s0165-1781(02)00249-4.
99. Hajak G, Rodenbeck A, Staedt J, Bandelow B, Huether G, Rüther E. 1995. Nocturnal plasma melatonin levels in patients suffering from chronic primary insomnia. Journal of Pineal Research. 19(3):116–122. doi:10.1111/j.1600-079x.1995.tb00179.x. http://dx.doi.org/10.1111/j.1600-079x.1995.tb00179.x.
100. Haimov I, Laudon M, Zisapel N, Souroujon M, Nof D, Shlitner A, Herer P, Tzischinsky O, Lavie P. 1994. Sleep disorders and melatonin rhythms in elderly people. BMJ. 309(6948):167–167. doi:10.1136/bmj.309.6948.167. http://dx.doi.org/10.1136/bmj.309.6948.167.
101. Cardinali DP, Srinivasan V, Brzezinski A, Brown GM. 2012. Melatonin and its analogs in insomnia and depression. Journal of Pineal Research. 52(4):365–375. doi:10.1111/j.1600-079x.2011.00962.x. http://dx.doi.org/10.1111/j.1600-079x.2011.00962.x.
102. Rodenbeck A, Huether G, Rüther E, Hajak G. 2002. Interactions between evening and nocturnal cortisol secretion and sleep parameters in patients with severe chronic primary insomnia. Neuroscience Letters. 324(2):159–163. doi:10.1016/s0304-3940(02)00192-1. http://dx.doi.org/10.1016/s0304-3940(02)00192-1.
103. Ohayon MM, Roth T. 2003. Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research. 37(1):9–15. doi:10.1016/s0022-3956(02)00052-3. http://dx.doi.org/10.1016/s0022-3956(02)00052-3.
104. Breslau N, Roth T, Rosenthal L, Andreski P. 1996. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young Adults. Biological Psychiatry. 39(6):411–418. doi:10.1016/0006-3223(95)00188-3. http://dx.doi.org/10.1016/0006-3223(95)00188-3.
105. Joseph JJ, Golden SH. 2016. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences. 1391(1):20–34. doi:10.1111/nyas.13217. http://dx.doi.org/10.1111/nyas.13217.
106. YoEargon M, Kara H, Solmaz M. 1997. Sleep Disturbances and Suicidal Behavior in Patients With Major Depression. The Journal of Clinical Psychiatry. 58(6):249–251. doi:10.4088/jcp.v58n0602. http://dx.doi.org/10.4088/jcp.v58n0602.
107. Kubatka P, Zubor P, Busselberg D, Kwon TK, Adamek M, Petrovic D, Opatrilova R, Gazdikova K, Caprnda M, Rodrigo L, et al. 2018. Melatonin and breast cancer: Evidences from preclinical and human studies. Critical Reviews in Oncology/Hematology. 122:133–143. doi:10.1016/j.critrevonc.2017.12.018. http://dx.doi.org/10.1016/j.critrevonc.2017.12.018.
108. Arbel I, Kadar T, Silbermann M, Levy A. 1994. The effects of long-term corticosterone administration on hippocampal morphology and cognitive performance of middle-aged rats. Brain Research. 657(1–2):227–235. doi:10.1016/0006-8993(94)90972-5. http://dx.doi.org/10.1016/0006-8993(94)90972-5.
109. Stokes PE. 1995. The potential role of excessive cortisol induced by HPA hyperfunction in the pathogenesis of depression. European Neuropsychopharmacology. 5:77–82. doi:10.1016/0924-977x(95)00039-r. http://dx.doi.org/10.1016/0924-977x(95)00039-r.
110. Lee AL, Ogle WO, Sapolsky RM. 2002. Stress and depression: possible links to neuron death in the hippocampus. Bipolar Disorders. 4(2):117–128. doi:10.1034/j.1399-5618.2002.01144.x. http://dx.doi.org/10.1034/j.1399-5618.2002.01144.x.
111. Ouanes S, Popp J. 2019. High Cortisol and the Risk of Dementia and Alzheimer’s Disease: A Review of the Literature. Frontiers in Aging Neuroscience. 11. doi:10.3389/fnagi.2019.00043. http://dx.doi.org/10.3389/fnagi.2019.00043.
112. Abell JG, Shipley MJ, Ferrie JE, Kivimäki M, Kumari M. 2016. Recurrent short sleep, chronic insomnia symptoms and salivary cortisol: A 10-year follow-up in the Whitehall II study. Psychoneuroendocrinology. 68:91–99. doi:10.1016/j.psyneuen.2016.02.021. http://dx.doi.org/10.1016/j.psyneuen.2016.02.021.
113. GUNNAR MR, VAZQUEZ DM. 2001. Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in humandevelopment. Development and Psychopathology. 13(3):515–538. doi:10.1017/s0954579401003066. http://dx.doi.org/10.1017/s0954579401003066.
114. Yehuda R, Seckl J. 2011. Minireview: Stress-Related Psychiatric Disorders with Low Cortisol Levels: A Metabolic Hypothesis. Endocrinology. 152(12):4496–4503. doi:10.1210/en.2011-1218. http://dx.doi.org/10.1210/en.2011-1218.
115. Salgado-Delgado R, Tapia Osorio A, Saderi N, Escobar C. 2011. Disruption of Circadian Rhythms: A Crucial Factor in the Etiology of Depression. Depression Research and Treatment. 2011:1–9. doi:10.1155/2011/839743. http://dx.doi.org/10.1155/2011/839743.
116. Leng Y, Musiek ES, Hu K, Cappuccio FP, Yaffe K. 2019. Association between circadian rhythms and neurodegenerative diseases. The Lancet Neurology. 18(3):307–318. doi:10.1016/s1474-4422(18)30461-7. http://dx.doi.org/10.1016/s1474-4422(18)30461-7.
117. Gery S, Koeffler HP. 2010. Circadian rhythms and cancer. Cell Cycle. 9(6):1097–1103. doi:10.4161/cc.9.6.11046. http://dx.doi.org/10.4161/cc.9.6.11046.
118. Parameswaran G, Ray DW. 2021. Sleep, circadian rhythms, and type 2 diabetes mellitus. Clinical Endocrinology. 96(1):12–20. doi:10.1111/cen.14607. http://dx.doi.org/10.1111/cen.14607.
119. Takeda N, Maemura K. 2011. Circadian clock and cardiovascular disease. Journal of Cardiology. 57(3):249–256. doi:10.1016/j.jjcc.2011.02.006. http://dx.doi.org/10.1016/j.jjcc.2011.02.006.
120. Lövheim H. 2012. A new three-dimensional model for emotions and monoamine neurotransmitters. Medical Hypotheses. 78(2):341–348. doi:10.1016/j.mehy.2011.11.016. http://dx.doi.org/10.1016/j.mehy.2011.11.016.
121. Megha K, Deshmukh PS, Ravi AK, Tripathi AK, Abegaonkar MP, Banerjee BD. 2015. Effect of Low-Intensity Microwave Radiation on Monoamine Neurotransmitters and Their Key Regulating Enzymes in Rat Brain. Cell Biochemistry and Biophysics. 73(1):93–100. doi:10.1007/s12013-015-0576-x. http://dx.doi.org/10.1007/s12013-015-0576-x.
122. Ismail S, Ali RF, Hassan HMM, Abdel-Rahman D. 2015. Effect of Exposure to Electromagnetic Fields (Emfs) on Monoamine Neurotransmitters of Newborn Rats. Biochemistry & Physiology: Open Access. 4(2). https://www.researchgate.net/publication/324227263.
123. Burchard JF, Nguyen DH, Richard L, Young SN, Heyes MP, Block E. 1998. Neurochemical Research. 23(12):1527–1531. doi:10.1023/a:1020975903631. http://dx.doi.org/10.1023/a:1020975903631.
124. Jain A, Mishra A, Shakkarpude J, Lakhani P. 2019. Beta endorphins: The natural opioids. Crescent Journal of Medical and Biological Sciences. 7(7):323–332. https://www.researchgate.net/publication/324569912.
125. Hestad K, Alexander J, Rootwelt H, Aaseth JO. 2022. The Role of Tryptophan Dysmetabolism and Quinolinic Acid in Depressive and Neurodegenerative Diseases. Biomolecules. 12(7):998. doi:10.3390/biom12070998. http://dx.doi.org/10.3390/biom12070998.
126. Brunner HG, Nelen M, Breakefield XO, Ropers HH, van Oost BA. 1993. Abnormal Behavior Associated with a Point Mutation in the Structural Gene for Monoamine Oxidase A. Science. 262(5133):578–580. doi:10.1126/science.8211186. http://dx.doi.org/10.1126/science.8211186.
127. Godar SC, Bortolato M, Castelli MP, Casti A, Casu A, Chen K, Ennas MG, Tambaro S, Shih JC. 2014. The aggression and behavioral abnormalities associated with monoamine oxidase A deficiency are rescued by acute inhibition of serotonin reuptake. Journal of Psychiatric Research. 56:1–9. doi:10.1016/j.jpsychires.2014.04.014. http://dx.doi.org/10.1016/j.jpsychires.2014.04.014.
128. Popova NK. 2008. From gene to aggressive behavior: The role of brain serotonin. Neuroscience and Behavioral Physiology. 38(5):471–475. doi:10.1007/s11055-008-9004-7. http://dx.doi.org/10.1007/s11055-008-9004-7.
129. Gvion Y, Apter A. 2011. Aggression, Impulsivity, and Suicide Behavior: A Review of the Literature. Archives of Suicide Research. 15(2):93–112. doi:10.1080/13811118.2011.565265. http://dx.doi.org/10.1080/13811118.2011.565265.
130. Träskman L. 1981. Monoamine Metabolites in CSF and Suicidal Behavior. Archives of General Psychiatry. 38(6):631. doi:10.1001/archpsyc.1981.01780310031002. http://dx.doi.org/10.1001/archpsyc.1981.01780310031002.
131. Brown GL, Ebert MH, Goyer PF, Jimerson DC, Klein WJ, Bunney WE, Goodwin FK. 1982. Aggression, suicide, and serotonin: relationships to CSF amine metabolites. The American journal of psychiatry. 139(6):741–6. doi:10.1176/ajp.139.6.741. [accessed 2024 Mar 17]. https://pubmed.ncbi.nlm.nih.gov/6177256/.
132. MANN JJ, ARANGO V, UNDERWOOD MD. 1990. Serotonin and Suicidal Behaviora. Annals of the New York Academy of Sciences. 600(1):476–484. doi:10.1111/j.1749-6632.1990.tb16903.x. http://dx.doi.org/10.1111/j.1749-6632.1990.tb16903.x.
133. Alvarez JC, Cremniter D, Lesieur P, Gregoire A, Gilton A, Macquin-Mavier I, Jarreau C, Spreux-Varoquaux O. 1999. Low blood cholesterol and low platelet serotonin levels in violent suicide attempters. Biological Psychiatry. 45(8):1066–1069. doi:10.1016/s0006-3223(98)00160-7. http://dx.doi.org/10.1016/s0006-3223(98)00160-7.
134. Placidi GP., Oquendo MA, Malone KM, Huang Y-Y, Ellis SP, Mann JJ. 2001. Aggressivity, suicide attempts, and depression: relationship to cerebrospinal fluid monoamine metabolite levels. Biological Psychiatry. 50(10):783–791. doi:10.1016/s0006-3223(01)01170-2. http://dx.doi.org/10.1016/s0006-3223(01)01170-2.
135. Delgado PL. 2000. Depression: the case for a monoamine deficiency. The Journal of clinical psychiatry. 61 Suppl 6:7–11. [accessed 2024 Mar 17]. https://pubmed.ncbi.nlm.nih.gov/10775018/.
136. Loo CK, Mitchell PB. 2005. A review of the efficacy of transcranial magnetic stimulation (TMS) treatment for depression, and current and future strategies to optimize efficacy. Journal of Affective Disorders. 88(3):255–267. doi:10.1016/j.jad.2005.08.001. http://dx.doi.org/10.1016/j.jad.2005.08.001.
137. Center for Brain Training. What is Neurofeedback? [accessed 2024 Mar 18]. https://www.centerforbrain.com/neurofeedback/what-is-neurofeedback/.
138. Ros T, Munneke MAM, Ruge D, Gruzelier JH, Rothwell JC. 2010. Endogenous control of waking brain rhythms induces neuroplasticity in humans. European Journal of Neuroscience. 31(4):770–778. doi:10.1111/j.1460-9568.2010.07100.x. http://dx.doi.org/10.1111/j.1460-9568.2010.07100.x.
139. World Health Organization. CI5plus CANCER INCIDENCE IN FIVE CONTINENTS TIME TRENDS. [accessed 2023 Nov 14]. https://ci5.iarc.who.int/ci5plus.
140. Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IB de O, Berti E, Bhagat G, Borges AM, Boyer D, Calaminici M, et al. 2022. The 5th edition of the World Health Organization Classification of Haematolymphoid Tumours: Lymphoid Neoplasms. Leukemia. 36(7):1720–1748. doi:10.1038/s41375-022-01620-2. http://dx.doi.org/10.1038/s41375-022-01620-2.
141. Michelozzi P. 2002. Adult and Childhood Leukemia near a High-Power Radio Station in Rome, Italy. American Journal of Epidemiology. 155(12):1096–1103. doi:10.1093/aje/155.12.1096. http://dx.doi.org/10.1093/aje/155.12.1096.
142. Dolk H, Shaddick G, Walls P, Grundy C, Thakrar B, Kleinschmidt I, Elliott P. 1997. Cancer Incidence near Radio and Television Transmitters in Great Britain I. Sutton Coldfield Transmitter. American Journal of Epidemiology. 145(1):1–9. doi:10.1093/oxfordjournals.aje.a009025. http://dx.doi.org/10.1093/oxfordjournals.aje.a009025.
143. SAVITZ DA, WACHTEL H, BARNES FA, JOHN EM, TVRDIK JG. 1988. CASE-CONTROL STUDY OF CHILDHOOD CANCER AND EXPOSURE TO 60-HZ MAGNETIC FIELDS. American Journal of Epidemiology. 128(1):21–38. doi:10.1093/oxfordjournals.aje.a114943. http://dx.doi.org/10.1093/oxfordjournals.aje.a114943.
144. Olsen JH, Nielsen A, Schulgen G. 1993. Residence near high voltage facilities and risk of cancer in children. BMJ. 307(6909):891–895. doi:10.1136/bmj.307.6909.891. http://dx.doi.org/10.1136/bmj.307.6909.891.
145. Schroeder JC, Savitz DA. 1997. Lymphoma and multiple myeloma mortality in relation to magnetic field exposure among electric utility workers. American Journal of Industrial Medicine. 32(4):392–402. doi:10.1002/(sici)1097-0274(199710)32:4<392::aid-ajim10>3.0.co;2-z. http://dx.doi.org/10.1002/(sici)1097-0274(199710)32:4<392::aid-ajim10>3.0.co;2-z.
146. Feychting M, Alhbom M. 1993. Magnetic Fields and Cancer in Children Residing Near Swedish High-voltage Power Lines. American Journal of Epidemiology. 138(7):467–481. doi:10.1093/oxfordjournals.aje.a116881. http://dx.doi.org/10.1093/oxfordjournals.aje.a116881.
147. Schüz J, Grigat J-P, Brinkmann K, Michaelis J. 2001. Residential magnetic fields as a risk factor for childhood acute leukaemia: Results from a German population-based case-control study. International Journal of Cancer. 91(5):728–735. doi:10.1002/1097-0215(200002)9999:9999<::aid-ijc1097>3.0.co;2-d. http://dx.doi.org/10.1002/1097-0215(200002)9999:9999<::aid-ijc1097>3.0.co;2-d.
148. Kabuto M, Nitta H, Yamamoto S, Yamaguchi N, Akiba S, Honda Y, Hagihara J, Isaka K, Saito T, Ojima T, et al. 2006. Childhood leukemia and magnetic fields in Japan: A case‐control study of childhood leukemia and residential power‐frequency magnetic fields in Japan. International Journal of Cancer. 119(3):643–650. doi:10.1002/ijc.21374. http://dx.doi.org/10.1002/ijc.21374.
149. Ogino K. 2019. Mi no Mawari no Denijha Hibaku (Exposure to Electromagnetic Radiation Around Us). [accessed 2023 Dec 26]. https://books.google.co.jp/books/about/%E8%BA%AB%E3%81%AE%E5%9B%9E%E3%82%8A%E3%81%AE%E9%9B%BB%E7%A3%81%E6%B3%A2%E8%A2%AB%E6%9B%9D.html?hl=&id=chqgwwEACAAJ&redir_esc=y.
150. Hatch EE, Linet MS, Kleinerman RA, Tarone RE, Severson RK, Hartsock CT, Haines C, Kaune WT, Friedman D, Robison LL, et al. 1998. Association between childhood acute lymphoblastic leukemia and use of electrical appliances during pregnancy and childhood. Epidemiology (Cambridge, Mass). 9(3):234–45. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/9583414/.
151. Hardell L, Eriksson M, Carlberg M, Sundström C, Mild KH. 2005. Use of cellular or cordless telephones and the risk for non-Hodgkin’s lymphoma. International Archives of Occupational and Environmental Health. 78(8):625–632. doi:10.1007/s00420-005-0003-5. http://dx.doi.org/10.1007/s00420-005-0003-5.
152. Draper G, Vincent T, Kroll ME, Swanson J. 2005. Childhood cancer in relation to distance from high voltage power lines in England and Wales: a case-control study. BMJ. 330(7503):1290. doi:10.1136/bmj.330.7503.1290. http://dx.doi.org/10.1136/bmj.330.7503.1290.
153. Hocking B, Gordon IR, Grain HL, Hatfield GE. 1996. Cancer incidence and mortality and proximity to TV towers. Medical Journal of Australia. 165(11–12):601–605. doi:10.5694/j.1326-5377.1996.tb138661.x. http://dx.doi.org/10.5694/j.1326-5377.1996.tb138661.x.
154. Floderus B, Törnqvist S, Stenlund C. 1994. Incidence of selected cancers in Swedish railway workers, 1961–79. Cancer Causes & Control. 5(2):189–194. doi:10.1007/bf01830265. http://dx.doi.org/10.1007/bf01830265.
155. Martínez JA. 2019. The “Moscow signal” epidemiological study, 40 years on. Reviews on Environmental Health. 34(1):13–24. doi:10.1515/reveh-2018-0061. http://dx.doi.org/10.1515/reveh-2018-0061.
156. healthline. What Do Leukemia Blood Counts Mean? [accessed 2023 Aug 5]. https://www.healthline.com/health/leukemia/leukemia-blood-count.
157. myleukemiateam. Low White Blood Cell Count and Leukemia. [accessed 2023 Jul 18]. https://www.myleukemiateam.com/resources/low-white-blood-cell-count-and-leukemia.
158. Alghamdi MS, El-Ghazaly NA. 2012. Effects of Exposure to Electromagnetic Field on of Some Hematological Parameters in Mice. Open Journal of Medicinal Chemistry. 02(02):30–42. doi:10.4236/ojmc.2012.22005. http://dx.doi.org/10.4236/ojmc.2012.22005.
159. El-Bediwi AB, Saad M, El-kott AF, Eid E. 2012. Influence of Electromagnetic Radiation Produced by Mobile Phone on Some Biophysical Blood Properties in Rats. Cell Biochemistry and Biophysics. 65(3):297–300. doi:10.1007/s12013-012-9432-4. http://dx.doi.org/10.1007/s12013-012-9432-4.
160. Jelodar G, Nazifi S, Nuhravesh M. 2010. Effect of electromagnetic field generated by BTS on hematological parameters and cellular composition of bone marrow in rat. Comparative Clinical Pathology. 20(6):551–555. doi:10.1007/s00580-010-1031-4. http://dx.doi.org/10.1007/s00580-010-1031-4.
161. Gandhi OP, Lazzi G, Furse CM. 1996. Electromagnetic absorption in the human head and neck for mobile telephones at 835 and 1900 MHz. IEEE Transactions on Microwave Theory and Techniques. 44(10):1884–1897. doi:10.1109/22.539947. http://dx.doi.org/10.1109/22.539947.
162. Persaud-Sharma D, Burns J, Trangle J, Moulik S. 2017. Disparities in Brain Cancer in the United States: A Literature Review of Gliomas. Medical Sciences. 5(3):16. doi:10.3390/medsci5030016. http://dx.doi.org/10.3390/medsci5030016.
163. Li K, Lu D, Guo Y, Wang C, Liu X, Liu Y, Liu D. 2018. Trends and patterns of incidence of diffuse glioma in adults in the United States, 1973‐2014. Cancer Medicine. 7(10):5281–5290. doi:10.1002/cam4.1757. http://dx.doi.org/10.1002/cam4.1757.
164. de Vocht F. 2016. Inferring the 1985–2014 impact of mobile phone use on selected brain cancer subtypes using Bayesian structural time series and synthetic controls. Environment International. 97:100–107. doi:10.1016/j.envint.2016.10.019. http://dx.doi.org/10.1016/j.envint.2016.10.019.
165. Aydin D, Feychting M, Schuz J, Tynes T, Andersen TV, Schmidt LS, Poulsen AH, Johansen C, Prochazka M, Lannering B, et al. 2011. Mobile Phone Use and Brain Tumors in Children and Adolescents: A Multicenter Case-Control Study. JNCI Journal of the National Cancer Institute. 103(16):1264–1276. doi:10.1093/jnci/djr244. http://dx.doi.org/10.1093/jnci/djr244.
166. Hardell L, Carlberg M, Mild KH. 2006. Case–control study of the association between the use of cellular and cordless telephones and malignant brain tumors diagnosed during 2000–2003. Environmental Research. 100(2):232–241. doi:10.1016/j.envres.2005.04.006. http://dx.doi.org/10.1016/j.envres.2005.04.006.
167. Hardell L, Carlberg M. 2015. Mobile phone and cordless phone use and the risk for glioma – Analysis of pooled case-control studies in Sweden, 1997–2003 and 2007–2009. Pathophysiology. 22(1):1–13. doi:10.1016/j.pathophys.2014.10.001. http://dx.doi.org/10.1016/j.pathophys.2014.10.001.
168. Carlberg M, Hardell L. 2014. Decreased Survival of Glioma Patients with Astrocytoma Grade IV (Glioblastoma Multiforme) Associated with Long-Term Use of Mobile and Cordless Phones. International Journal of Environmental Research and Public Health. 11(10):10790–10805. doi:10.3390/ijerph111010790. http://dx.doi.org/10.3390/ijerph111010790.
169. Johnson DR, O’Neill BP. 2011. Glioblastoma survival in the United States before and during the temozolomide era. Journal of Neuro-Oncology. 107(2):359–364. doi:10.1007/s11060-011-0749-4. http://dx.doi.org/10.1007/s11060-011-0749-4.
170. Claus EB, Walsh KM, Wiencke JK, Molinaro AM, Wiemels JL, Schildkraut JM, Bondy ML, Berger M, Jenkins R, Wrensch M. 2015. Survival and low-grade glioma: the emergence of genetic information. Neurosurgical Focus. 38(1):E6. doi:10.3171/2014.10.focus12367. http://dx.doi.org/10.3171/2014.10.focus12367.
171. Carlberg M, Koppel T, Ahonen M, Hardell L. 2017. Case‐control study on occupational exposure to extremely low‐frequency electromagnetic fields and glioma risk. American Journal of Industrial Medicine. 60(5):494–503. doi:10.1002/ajim.22707. http://dx.doi.org/10.1002/ajim.22707.
172. HARDELL L, CARLBERG M, SÖDERQVIST F, MILD KH. 2013. Pooled analysis of case-control studies on acoustic neuroma diagnosed 1997–2003 and 2007–2009 and use of mobile and cordless phones. International Journal of Oncology. 43(4):1036–1044. doi:10.3892/ijo.2013.2025. http://dx.doi.org/10.3892/ijo.2013.2025.
173. Coureau G, Bouvier G, Lebailly P, Fabbro-Peray P, Gruber A, Leffondre K, Guillamo J-S, Loiseau H, Mathoulin-Pélissier S, Salamon R, et al. 2014. Mobile phone use and brain tumours in the CERENAT case-control study. Occupational and Environmental Medicine. 71(7):514–522. doi:10.1136/oemed-2013-101754. http://dx.doi.org/10.1136/oemed-2013-101754.
174. CARLBERG M, HARDELL L. 2015. Pooled analysis of Swedish case-control studies during 1997–2003 and 2007–2009 on meningioma risk associated with the use of mobile and cordless phones. Oncology Reports. 33(6):3093–3098. doi:10.3892/or.2015.3930. http://dx.doi.org/10.3892/or.2015.3930.
175. Savitz DA, Loomis DP. 1995. Magnetic Field Exposure in Relation to Leukemia and Brain Cancer Mortality among Electric Utility Workers. American Journal of Epidemiology. 141(2):123–134. doi:10.1093/oxfordjournals.aje.a117400. http://dx.doi.org/10.1093/oxfordjournals.aje.a117400.
176. Speers MA, Dobbins JG, Miller VS. 1988. Occupational exposures and brain cancer mortality: A preliminary study of East Texas residents. American Journal of Industrial Medicine. 13(6):629–638. doi:10.1002/ajim.4700130603. http://dx.doi.org/10.1002/ajim.4700130603.
177. Lin RS, Dischinger PC, Conde J, Farrell KP. 1985. Occupational exposure to electromagnetic fields and the occurrence of brain tumors. An analysis of possible associations. Journal of occupational medicine : official publication of the Industrial Medical Association. 27(6):413–9. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/4020499/.
178. Sadetzki S, Chetrit A, Jarus-Hakak A, Cardis E, Deutch Y, Duvdevani S, Zultan A, Novikov I, Freedman L, Wolf M. 2008. Cellular Phone Use and Risk of Benign and Malignant Parotid Gland Tumors--A Nationwide Case-Control Study. American Journal of Epidemiology. 167(4):457–467. doi:10.1093/aje/kwm325. http://dx.doi.org/10.1093/aje/kwm325.
179. Gombos A. 2019. Selective oestrogen receptor degraders in breast cancer: a review and perspectives. Current Opinion in Oncology. 31(5):424–429. doi:10.1097/cco.0000000000000567. http://dx.doi.org/10.1097/cco.0000000000000567.
180. Anderson WF, Katki HA, Rosenberg PS. 2011. Incidence of Breast Cancer in the United States: Current and Future Trends. JNCI Journal of the National Cancer Institute. 103(18):1397–1402. doi:10.1093/jnci/djr257. http://dx.doi.org/10.1093/jnci/djr257.
181. Shih Y-W, Hung C-S, Huang C-C, Chou K-R, Niu S-F, Chan S, Tsai H-T. 2020. <p>The Association Between Smartphone Use and Breast Cancer Risk Among Taiwanese Women: A Case-Control Study</p> Cancer Management and Research. Volume 12:10799–10807. doi:10.2147/cmar.s267415. http://dx.doi.org/10.2147/cmar.s267415.
182. Zhu K. 2003. Use of Electric Bedding Devices and Risk of Breast Cancer in African-American Women. American Journal of Epidemiology. 158(8):798–806. doi:10.1093/aje/kwg220. http://dx.doi.org/10.1093/aje/kwg220.
183. Feychting M, Forssén U, Rutqvist LE, Ahlbom A. 1998. Magnetic fields and breast cancer in Swedish adults residing near high-voltage power lines. Epidemiology (Cambridge, Mass). 9(4):392–7. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/9647902/.
184. Kliukiene J, Tynes T, Andersen A. 2003. Follow-up of radio and telegraph operators with exposure to electromagnetic fields and risk of breast cancer. European Journal of Cancer Prevention. 12(4):301–307. doi:10.1097/00008469-200308000-00010. http://dx.doi.org/10.1097/00008469-200308000-00010.
185. Demers PA, Thomas DB, Rosenblatt KA, Jimenez LM, McTiernan A, Stalsberg H, Stemhagen A, Thompson WD, Curnen MGM, Satariano W, et al. 1991. Occupational Exposure to Electromagnetic Fields and Breast Cancer in Men. American Journal of Epidemiology. 134(4):340–347. doi:10.1093/oxfordjournals.aje.a116095. http://dx.doi.org/10.1093/oxfordjournals.aje.a116095.
186. Coogan PF, Clapp RW, Newcomb PA, Wenzl TB, Bogdan G, Mittendorf R, Baron JA, Longnecker MP. 1996. Occupational exposure to 60-hertz magnetic fields and risk of breast cancer in women. Epidemiology (Cambridge, Mass). 7(5):459–64. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/8862974/.
187. Van Wijngaarden E, Nylander-French LA, Millikan RC, Savitz DA, Loomis D. 2001. Population-Based Case-Control Study of Occupational Exposure to Electromagnetic Fields and Breast Cancer. Annals of Epidemiology. 11(5):297–303. doi:10.1016/s1047-2797(01)00209-5. http://dx.doi.org/10.1016/s1047-2797(01)00209-5.
188. Loomis DP, Savitz DA, Ananth CV. 1994. Breast Cancer Mortality Among Female Electrical Workers in the United States. JNCI Journal of the National Cancer Institute. 86(12):921–925. doi:10.1093/jnci/86.12.921. http://dx.doi.org/10.1093/jnci/86.12.921.
189. Singh SR, Burnicka-Turek O, Chauhan C, Hou SX. 2011. Spermatogonial stem cells, infertility and testicular cancer. Journal of Cellular and Molecular Medicine. 15(3):468–483. doi:10.1111/j.1582-4934.2010.01242.x. http://dx.doi.org/10.1111/j.1582-4934.2010.01242.x.
190. Ramón y Cajal S, Sesé M, Capdevila C, Aasen T, De Mattos-Arruda L, Diaz-Cano SJ, Hernández-Losa J, Castellví J. 2020. Clinical implications of intratumor heterogeneity: challenges and opportunities. Journal of Molecular Medicine. 98(2):161–177. doi:10.1007/s00109-020-01874-2. http://dx.doi.org/10.1007/s00109-020-01874-2.
191. Chia VM, Quraishi SM, Devesa SS, Purdue MP, Cook MB, McGlynn KA. 2010. International Trends in the Incidence of Testicular Cancer, 1973-2002. Cancer Epidemiology, Biomarkers & Prevention. 19(5):1151–1159. doi:10.1158/1055-9965.epi-10-0031. http://dx.doi.org/10.1158/1055-9965.epi-10-0031.
192. Stenlund C, Floderus B. 1997. Cancer Causes and Control. 8(2):184–191. doi:10.1023/a:1018468112964. http://dx.doi.org/10.1023/a:1018468112964.
193. Hardell L, Carlberg M, Ohlson C ‐G., Westberg H, Eriksson M, Hansson Mild K. 2006. Use of cellular and cordless telephones and risk of testicular cancer. International Journal of Andrology. 30(2):115–122. doi:10.1111/j.1365-2605.2006.00721.x. http://dx.doi.org/10.1111/j.1365-2605.2006.00721.x.
194. Davis RL, Mostofi FK. 1993. Cluster of testicular cancer in police officers exposed to hand‐held radar. American Journal of Industrial Medicine. 24(2):231–233. doi:10.1002/ajim.4700240209. http://dx.doi.org/10.1002/ajim.4700240209.
195. Baumgardt-Elms C, Sch�mann M, Ahrens W, Bromen K, Stang A, Jahn I, Stegmaier C, J�ckel K-H. 2004. Residential exposure to overhead high-voltage lines and the risk of testicular cancer: results of a population-based case?control study in Hamburg (Germany). International Archives of Occupational and Environmental Health. 78(1):20–26. doi:10.1007/s00420-004-0550-1. http://dx.doi.org/10.1007/s00420-004-0550-1.
196. VERREAULT R, WEISS NS, HOLLENBACH KA, STRADER CH, DALING JR. 1990. USE OF ELECTRIC BLANKETS AND RISK OF TESTICULAR CANCER. American Journal of Epidemiology. 131(5):759–762. doi:10.1093/oxfordjournals.aje.a115565. http://dx.doi.org/10.1093/oxfordjournals.aje.a115565.
197. Eger H, Hagen KU, Lucas B, Voge P, Voit Helmut. 2004. The Influence of Being Physically Near to a Cell Phone Transmission Mast on the Incidence of Cancer. Umwelt Medizin Gesellschaft. 17(4). https://www.researchgate.net/publication/241473738.
198. Wolf R, Wolf D. 2004. Increased incidence of cancer near a cell-phone transmitter station. International Journal of Cancer Prevention. 1(2). https://www.researchgate.net/publication/228490892.
199. Tomenius L. 1986. 50‐Hz electromagnetic environment and the incidence of childhood tumors in Stockholm county. Bioelectromagnetics. 7(2):191–207. doi:10.1002/bem.2250070209. http://dx.doi.org/10.1002/bem.2250070209.
200. Armstrong B, Thériault G, Guénel P, Deadman J, Goldberg M, Héroux P. 1994. Association between Exposure to Pulsed Electromagnetic Fields and Cancer in Electric Utility Workers in Quebec, Canada, and France. American Journal of Epidemiology. 140(9):805–820. doi:10.1093/oxfordjournals.aje.a117329. http://dx.doi.org/10.1093/oxfordjournals.aje.a117329.
201. De Roos AJ, Teschke K, Savitz DA, Poole C, Grufferman S, Pollock BH, Olshan AF. 2001. Parental Occupational Exposures to Electromagnetic Fields and Radiation and the Incidence of Neuroblastoma in Offspring. Epidemiology. 12(5):508–517. doi:10.1097/00001648-200109000-00008. http://dx.doi.org/10.1097/00001648-200109000-00008.
202. Ji B-T, Silverman DT, Dosemeci M, Dai Q, Gao Y-T, Blair A. 1999. Occupation and pancreatic cancer risk in Shanghai, China. American Journal of Industrial Medicine. 35(1):76–81. doi:10.1002/(sici)1097-0274(199901)35:1<76::aid-ajim10>3.0.co;2-6. http://dx.doi.org/10.1002/(sici)1097-0274(199901)35:1<76::aid-ajim10>3.0.co;2-6.
203. Hardell L, Carlberg M, Hansson Mild K, Eriksson M. 2011. Case-control study on the use of mobile and cordless phones and the risk for malignant melanoma in the head and neck region. Pathophysiology. 18(4):325–333. doi:10.1016/j.pathophys.2011.06.001. http://dx.doi.org/10.1016/j.pathophys.2011.06.001.
204. Stang A, Anastassiou G, Ahrens W, Bromen K, Bornfeld N, Jöckel K-H. 2001. The Possible Role of Radiofrequency Radiation in the Development of Uveal Melanoma. Epidemiology. 12(1):7–12. doi:10.1097/00001648-200101000-00003. http://dx.doi.org/10.1097/00001648-200101000-00003.
205. Charles LE. 2003. Electromagnetic Fields, Polychlorinated Biphenyls, and Prostate Cancer Mortality in Electric Utility Workers. American Journal of Epidemiology. 157(8):683–691. doi:10.1093/aje/kwg044. http://dx.doi.org/10.1093/aje/kwg044.
206. SPITZ MR, JOHNSON CC. 1985. NEUROBLASTOMA AND PATERNAL OCCUPATION A CASE-CONTROL ANALYSIS. American Journal of Epidemiology. 121(6):924–929. doi:10.1093/oxfordjournals.aje.a114062. http://dx.doi.org/10.1093/oxfordjournals.aje.a114062.
207. Weiderpass E, Vainio H, Kauppinen T, Vasama-Neuvonen K, Partanen T, Pukkala E. 2003. Occupational Exposures and Gastrointestinal Cancers Among Finnish Women. Journal of Occupational and Environmental Medicine. 45(3):305–315. doi:10.1097/01.jom.0000052963.43131.44. http://dx.doi.org/10.1097/01.jom.0000052963.43131.44.
208. Zhu K, Weiss NS, Stanford JL, Daling JR, Stergachis A, McKnight B, Brawer MK, Levine RS. 1999. Prostate cancer in relation to the use of electric blanket or heated water bed. Epidemiology (Cambridge, Mass). 10(1):83–5. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/9888286/.
209. Holly EA, Aston DA, Ahm DK, Smith AH. 1996. Intraocular Melanoma Linked to Occupations and Chemical Exposures. Epidemiology. 7(1):55–61. doi:10.1097/00001648-199601000-00010. http://dx.doi.org/10.1097/00001648-199601000-00010.
210. Behrens T, Lynge E, Cree I, Sabroe S, Lutz J-M, Afonso N, Eriksson M, Guenel P, Merletti F, Morales-Suarez-Varela M, et al. 2010. Occupational exposure to electromagnetic fields and sex-differential risk of uveal melanoma. Occupational and Environmental Medicine. 67(11):751–759. doi:10.1136/oem.2009.052225. http://dx.doi.org/10.1136/oem.2009.052225.
211. Szmigielski S, Szudzinski A, Pietraszek A, Bielec M, Janiak M, Wrembel JK. 1982. Accelerated development of spontaneous and benzopyrene‐induced skin cancer in mice exposed to 2450‐MHz microwave radiation. Bioelectromagnetics. 3(2):179–191. doi:10.1002/bem.2250030202. http://dx.doi.org/10.1002/bem.2250030202.
212. Chou C ‐K., Guy AW, Kunz LL, Johnson RB, Crowley JJ, Krupp JH. 1992. Long‐term, low‐level microwave irradiation of rats. Bioelectromagnetics. 13(6):469–496. doi:10.1002/bem.2250130605. http://dx.doi.org/10.1002/bem.2250130605.
213. Löscher W, Mevissen M, Lehmacher W, Stamm A. 1993. Tumor promotion in a breast cancer model by exposure to a weak alternating magnetic field. Cancer Letters. 71(1–3):75–81. doi:10.1016/0304-3835(93)90100-n. http://dx.doi.org/10.1016/0304-3835(93)90100-n.
214. Repacholi MH, Basten A, Gebski V, Noonan D, Finnie J, Harris AW. 1997. Lymphomas in Eμ-Pim1 Transgenic Mice Exposed to Pulsed 900 MHz Electromagnetic Fields. Radiation Research. 147(5):631. doi:10.2307/3579630. http://dx.doi.org/10.2307/3579630.
215. Fam WZ, Mikhail EL. 1996. Lymphoma induced in mice chronically exposed to very strong low-frequency electromagnetic field. Cancer Letters. 105(2):257–269. doi:10.1016/0304-3835(96)04324-8. http://dx.doi.org/10.1016/0304-3835(96)04324-8.
216. Levine H, Jørgensen N, Martino-Andrade A, Mendiola J, Weksler-Derri D, Jolles M, Pinotti R, Swan SH. 2022. Temporal trends in sperm count: a systematic review and meta-regression analysis of samples collected globally in the 20th and 21st centuries. Human Reproduction Update. 29(2):157–176. doi:10.1093/humupd/dmac035. http://dx.doi.org/10.1093/humupd/dmac035.
217. CDC. Archived ART Reports, Spreadsheets and Surveillance Summaries. [accessed 2023 Nov 21]. https://www.cdc.gov/art/reports/archive.html.
218. Japan Society of Obstetrics and Gynecology. ART Databook for 2019. [accessed 2023 Jun 21]. https://www.jsog.or.jp/modules/committee/index.php?content_id=12.
219. International Clearinghouse for Birth Defects Surveillance and Research. Annual Report 2013. [accessed 2023 Jun 21]. http://www.icbdsr.org/resources/annual-report/.
220. Lang K, Nuevo-Chiquero A. 2012. Trends in Self-reported Spontaneous Abortions: 1970–2000. Demography. 49(3):989–1009. doi:10.1007/s13524-012-0113-0. http://dx.doi.org/10.1007/s13524-012-0113-0.
221. Adolfsson A. 2006. Miscarriage: women’s experience and its cumulative incidence. [accessed 2023 Jan 17]. https://books.google.co.jp/books/about/Miscarriage.html?hl=&id=Ei0wNgAACAAJ&redir_esc=y.
222. CDC WONDER. Natality Information Live Births. [accessed 2023 Nov 21]. https://wonder.cdc.gov/natality.html.
223. Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller A-B, Narwal R, Adler A, Vera Garcia C, Rohde S, Say L, et al. 2012. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. The Lancet. 379(9832):2162–2172. doi:10.1016/s0140-6736(12)60820-4. http://dx.doi.org/10.1016/s0140-6736(12)60820-4.
224. Davis DL, Gottlieb MB, Stampnitzky JR. 1998. Reduced Ratio of Male to Female Births in Several Industrial Countries. JAMA. 279(13):1018. doi:10.1001/jama.279.13.1018. http://dx.doi.org/10.1001/jama.279.13.1018.
225. Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. 2008. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study. Fertility and Sterility. 89(1):124–128. doi:10.1016/j.fertnstert.2007.01.166. http://dx.doi.org/10.1016/j.fertnstert.2007.01.166.
226. Ding S-S, Sun P, Tian H, Huo Y-W, Wang L-R, Han Y, Zhang Z, Liu X, Xing J-P. 2018. Association between daily exposure to electromagnetic radiation from 4G smartphone and 2.45-GHz wi-fi and oxidative damage to semen of males attending a genetics clinic: a primary study. International Journal of Clinical and Experimental Medicine. 11(3):2821–2830. https://www.ijcem.com/files/ijcem0063001.pdf.
227. Kilgallon SJ, Simmons LW. 2005. Image content influences men’s semen quality. Biology Letters. 1(3):253–255. doi:10.1098/rsbl.2005.0324. http://dx.doi.org/10.1098/rsbl.2005.0324.
228. Fejes I, Závaczki Z, Szöllősi J, Koloszár S, Daru J, Kovács L, Pál A. 2005. IS THERE A RELATIONSHIP BETWEEN CELL PHONE USE AND SEMEN QUALITY? Archives of Andrology. 51(5):385–393. doi:10.1080/014850190924520. http://dx.doi.org/10.1080/014850190924520.
229. El-Helaly M, Awadalla N, Mansour M, El-Biomy Y. 2010. Workplace exposures and male infertility - a case-control study. International journal of occupational medicine and environmental health. 23(4):331–8. doi:10.2478/v10001-010-0039-y. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/21306978/.
230. Otitoloju AA, Obe IA, Adewale OA, Otubanjo OA, Osunkalu VO. 2009. Preliminary Study on the Induction of Sperm Head Abnormalities in Mice, Mus musculus, Exposed to Radiofrequency Radiations from Global System for Mobile Communication Base Stations. Bulletin of Environmental Contamination and Toxicology. 84(1):51–54. doi:10.1007/s00128-009-9894-2. http://dx.doi.org/10.1007/s00128-009-9894-2.
231. Kumar N, Singh A. 2015. Trends of male factor infertility, an important cause of infertility: A review of literature. Journal of Human Reproductive Sciences. 8(4):191. doi:10.4103/0974-1208.170370. http://dx.doi.org/10.4103/0974-1208.170370.
232. Bin-Meferij MM, El-Kott AF. 2015. The radioprotective effects of Moringa oleifera against mobile phone electromagnetic radiation-induced infertility in rats. International journal of clinical and experimental medicine. 8(8):12487–97. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/26550159/.
233. McNally AK, Anderson JM. 2011. Macrophage Fusion and Multinucleated Giant Cells of Inflammation. Advances in Experimental Medicine and Biology.:97–111. doi:10.1007/978-94-007-0763-4_7. http://dx.doi.org/10.1007/978-94-007-0763-4_7.
234. Pandey N, Giri S, Das S, Upadhaya P. 2016. Radiofrequency radiation (900 MHz)-induced DNA damage and cell cycle arrest in testicular germ cells in swiss albino mice. Toxicology and Industrial Health. 33(4):373–384. doi:10.1177/0748233716671206. http://dx.doi.org/10.1177/0748233716671206.
235. Kumar S, Nirala JP, Behari J, Paulraj R. 2014. Effect of electromagnetic irradiation produced by 3G mobile phone on male rat reproductive system in a simulated scenario. Indian journal of experimental biology. 52(9):890–7. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/25241589/.
236. Esmailzadeh S, Delavar MA, Aleyassin A, Gholamian SA, Ahmadi A. 2019. Exposure to Electromagnetic Fields of High Voltage Overhead Power Lines and Female Infertility. The international journal of occupational and environmental medicine. 10(1):11–16. doi:10.15171/ijoem.2019.1429. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/30685773/.
237. SUGINO N. 2005. Reactive oxygen species in ovarian physiology. Reproductive Medicine and Biology. 4(1):31–44. doi:10.1111/j.1447-0578.2005.00086.x. http://dx.doi.org/10.1111/j.1447-0578.2005.00086.x.
238. Yao W, Pan Z, Du X, Zhang J, Liu H, Li Q. 2021. NORHA, a novel follicular atresia-related lncRNA, promotes porcine granulosa cell apoptosis via the miR-183-96-182 cluster and FoxO1 axis. Journal of Animal Science and Biotechnology. 12(1). doi:10.1186/s40104-021-00626-7. http://dx.doi.org/10.1186/s40104-021-00626-7.
239. İdil M, Çepni İ, Demirsoy G, Öcal P, Salihoğlu F, Şenol H, Elibol F, İrez T. 2004. Does granulosa cell apoptosis have a role in the etiology of unexplained infertility? European Journal of Obstetrics & Gynecology and Reproductive Biology. 112(2):182–184. doi:10.1016/s0301-2115(03)00365-8. http://dx.doi.org/10.1016/s0301-2115(03)00365-8.
240. Türedi S, Hancı H, Çolakoğlu S, Kaya H, Odacı E. 2016. Disruption of the ovarian follicle reservoir of prepubertal rats following prenatal exposure to a continuous 900-MHz electromagnetic field. International Journal of Radiation Biology. 92(6):329–337. doi:10.3109/09553002.2016.1152415. http://dx.doi.org/10.3109/09553002.2016.1152415.
241. Rad Js, Roshangar L, Hamdi B, Khaki A, Soleimani-Rad S. 2014. Effect of low-frequency electromagnetic field exposure on oocyte differentiation and follicular development. Advanced Biomedical Research. 3(1):76. doi:10.4103/2277-9175.125874. http://dx.doi.org/10.4103/2277-9175.125874.
242. Bakacak M, Bostancı MS, Attar R, Yıldırım ÖK, Yıldırım G, Bakacak Z, Sayar H, Han A. 2015. The effects of electromagnetic fields on the number of ovarian primordial follicles: An experimental study. The Kaohsiung Journal of Medical Sciences. 31(6):287–292. doi:10.1016/j.kjms.2015.03.004. http://dx.doi.org/10.1016/j.kjms.2015.03.004.
243. Panagopoulos DJ, Chavdoula ED, Margaritis LH. 2010. Bioeffects of mobile telephony radiation in relation to its intensity or distance from the antenna. International Journal of Radiation Biology. 86(5):345–357. doi:10.3109/09553000903567961. http://dx.doi.org/10.3109/09553000903567961.
244. Gul A, Çelebi H, Uğraş S. 2009. The effects of microwave emitted by cellular phones on ovarian follicles in rats. Archives of Gynecology and Obstetrics. 280(5):729–733. doi:10.1007/s00404-009-0972-9. http://dx.doi.org/10.1007/s00404-009-0972-9.
245. Khaki A. 2013. Effect of Ocimum basilicum on ovary tissue histopathology after exposure to electromagnetic fields (EMF) in rats. African Journal of Pharmacy and Pharmacology. 7(25):1703–1706. doi:10.5897/ajpp12.1073. http://dx.doi.org/10.5897/ajpp12.1073.
246. Mahmoudabadi FS, Ziaei S, Firoozabadi M, Kazemnejad A. 2015. Use of mobile phone during pregnancy and the risk of spontaneous abortion. Journal of Environmental Health Science and Engineering. 13(1). doi:10.1186/s40201-015-0193-z. http://dx.doi.org/10.1186/s40201-015-0193-z.
247. Zhou L, Zhang H, Lan Y, Li Y, Liang Y, Yu L, Ma Y, Jia C, Wang S. 2015. Epidemiological investigation of risk factors of the pregnant women with early spontaneous abortion in Beijing. Chinese Journal of Integrative Medicine. 23(5):345–349. doi:10.1007/s11655-015-2144-z. http://dx.doi.org/10.1007/s11655-015-2144-z.
248. Wang Q, Cao Z, Qu Y, Peng X, Guo S, Chen L. 2013. Residential Exposure to 50 Hz Magnetic Fields and the Association with Miscarriage Risk: A 2-Year Prospective Cohort Study. Frasch MG, editor. PLoS ONE. 8(12):e82113. doi:10.1371/journal.pone.0082113. http://dx.doi.org/10.1371/journal.pone.0082113.
249. Li D-K, Chen H, Ferber JR, Odouli R, Quesenberry C. 2017. Exposure to Magnetic Field Non-Ionizing Radiation and the Risk of Miscarriage: A Prospective Cohort Study. Scientific Reports. 7(1). doi:10.1038/s41598-017-16623-8. http://dx.doi.org/10.1038/s41598-017-16623-8.
250. Goldhaber MK, Fireman BH. 1991. The fetal life table revisited: spontaneous abortion rates in three Kaiser Permanente cohorts. Epidemiology (Cambridge, Mass). 2(1):33–9. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/2021664/.
251. Juutilainen J, Matilainen P, Saarikoski S, Läärä E, Suonio S. 1993. Early pregnancy loss and exposure to 50‐Hz magnetic fields. Bioelectromagnetics. 14(3):229–236. doi:10.1002/bem.2250140306. http://dx.doi.org/10.1002/bem.2250140306.
252. Belanger K, Leaderer B, Hellenbrand K, Holford TR, McSharry J, Power ME, Bracken MB. 1998. Spontaneous abortion and exposure to electric blankets and heated water beds. Epidemiology (Cambridge, Mass). 9(1):36–42. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/9430266/.
253. Shamsi Mahmoudabadi F, Ziaei S, Firoozabadi M, Kazemnejad A. 2013. Exposure to extremely low frequency electromagnetic fields during pregnancy and the risk of spontaneous abortion: a case-control study. Journal of research in health sciences. 13(2):131–4. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/24077469/.
254. Mohebi M, Ghafouri-Fard S. 2019. Embryo developmental arrest: Review of genetic factors and pathways. Gene Reports. 17:100479. doi:10.1016/j.genrep.2019.100479. http://dx.doi.org/10.1016/j.genrep.2019.100479.
255. Hardy K. 1999. Apoptosis in the human embryo. Reviews of Reproduction. 4(3):125–134. doi:10.1530/ror.0.0040125. http://dx.doi.org/10.1530/ror.0.0040125.
256. Balaban B, Urman B, Sertac A, Alatas C, Aksoy S, Mercan R. 2000. Blastocyst quality affects the success of blastocyst-stage embryo transfer. Fertility and Sterility. 74(2):282–287. doi:10.1016/s0015-0282(00)00645-2. http://dx.doi.org/10.1016/s0015-0282(00)00645-2.
257. Seshagiri PB, Sen Roy S, Sireesha G, Rao RP. 2009. Cellular and molecular regulation of mammalian blastocyst hatching. Journal of Reproductive Immunology. 83(1–2):79–84. doi:10.1016/j.jri.2009.06.264. http://dx.doi.org/10.1016/j.jri.2009.06.264.
258. Hassold T, Hunt P. 2001. To err (meiotically) is human: the genesis of human aneuploidy. Nature Reviews Genetics. 2(4):280–291. doi:10.1038/35066065. http://dx.doi.org/10.1038/35066065.
259. Safian F, Khalili MA, Khoradmehr A, Anbari F, Soltani S, Halvaei I. 2016. Survival Assessment of Mouse Preimplantation Embryos After Exposure to Cell Phone Radiation. Journal of reproduction & infertility. 17(3):138–43. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/27478766/.
260. Borhani N, Rajaei F, Salehi Z, Javadi A. 2011. Analysis of DNA fragmentation in mouse embryos exposed to an extremely low-frequency electromagnetic field. Electromagnetic Biology and Medicine. 30(4):246–252. doi:10.3109/15368378.2011.589556. http://dx.doi.org/10.3109/15368378.2011.589556.
261. Alchalabi ASH, Aklilu E, Aziz AR, Malek F, Ronald SH, Khan MA. 2016. Different periods of intrauterine exposure to electromagnetic field: Influence on female rats’ fertility, prenatal and postnatal development. Asian Pacific Journal of Reproduction. 5(1):14–23. doi:10.1016/j.apjr.2015.12.003. http://dx.doi.org/10.1016/j.apjr.2015.12.003.
262. Magras IN, Xenos TD. 1997. RF radiation-induced changes in the prenatal development of mice. Bioelectromagnetics. 18(6):455–461. doi:10.1002/(sici)1521-186x(1997)18:6<455::aid-bem8>3.0.co;2-1. http://dx.doi.org/10.1002/(sici)1521-186x(1997)18:6<455::aid-bem8>3.0.co;2-1.
263. Balmori A. 2005. Possible Effects of Electromagnetic Fields from Phone Masts on a Population of White Stork (Ciconia ciconia). Electromagnetic Biology and Medicine. 24(2):109–119. doi:10.1080/15368370500205472. http://dx.doi.org/10.1080/15368370500205472.
264. Al‐Akhras M, Elbetieha A, Hasan M, Al‐Omari I, Darmani H, Albiss B. 2001. Effects of extremely low frequency magnetic field on fertility of adult male and female rats. Bioelectromagnetics. 22(5):340–344. doi:10.1002/bem.59. http://dx.doi.org/10.1002/bem.59.
265. Ericson A, Källén B. 1986. An epidemiological study of work with video screens and pregnancy outcome: II. A case–control study. American Journal of Industrial Medicine. 9(5):459–475. doi:10.1002/ajim.4700090507. http://dx.doi.org/10.1002/ajim.4700090507.
266. Nordström S, Birke E, Gustavsson L. 1983. Reproductive hazards among workers at high voltage substations. Bioelectromagnetics. 4(1):91–101. doi:10.1002/bem.2250040109. http://dx.doi.org/10.1002/bem.2250040109.
267. Li D-K, Checkoway H, Mueller BA. 1995. Electric Blanket Use during Pregnancy in Relation to the Risk of Congenital Urinary Tract Anomalies among Women with a History of Subfertility. Epidemiology. 6(5):485–489. doi:10.1097/00001648-199509000-00004. http://dx.doi.org/10.1097/00001648-199509000-00004.
268. Stonebrook E, Hoff M, Spencer JD. 2019. Congenital Anomalies of the Kidney and Urinary Tract: a Clinical Review. Current Treatment Options in Pediatrics. 5(3):223–235. doi:10.1007/s40746-019-00166-3. http://dx.doi.org/10.1007/s40746-019-00166-3.
269. Becker RO, Becker AJ. 1986. An Analysis of the Effectiveness of Regulatory Agency Responses to a Situation Involving Perceived Health Effects from Microwave Radiation. Journal of Bioelectricity. 5(2):229–251. doi:10.1080/15368378609006059. http://dx.doi.org/10.1080/15368378609006059.
270. Wertheimer N, Leeper E. 1986. Possible effects of electric blankets and heated waterbeds on fetal development. Bioelectromagnetics. 7(1):13–22. doi:10.1002/bem.2250070103. http://dx.doi.org/10.1002/bem.2250070103.
271. Goldhaber MK, Polen MR, Hiatt RA. 1988. The risk of miscarriage and birth defects among women who use visual display terminals during pregnancy. American Journal of Industrial Medicine. 13(6):695–706. doi:10.1002/ajim.4700130608. http://dx.doi.org/10.1002/ajim.4700130608.
272. Augustianath T, Evans DA, Anisha GS. 2023. Teratogenic effects of radiofrequency electromagnetic radiation on the embryonic development of chick: A study on morphology and hatchability. Research in Veterinary Science. 159:93–100. doi:10.1016/j.rvsc.2023.04.015. http://dx.doi.org/10.1016/j.rvsc.2023.04.015.
273. Cleveland Clinic. Low Birth Weight. [accessed 2023 Aug 26]. https://my.clevelandclinic.org/health/diseases/24980-low-birth-weight.
274. de Vocht F, Hannam K, Baker P, Agius R. 2014. Maternal residential proximity to sources of extremely low frequency electromagnetic fields and adverse birth outcomes in a UK cohort. Bioelectromagnetics. 35(3):201–209. doi:10.1002/bem.21840. http://dx.doi.org/10.1002/bem.21840.
275. Lu X, Oda M, Ohba T, Mitsubuchi H, Masuda S, Katoh T. 2017. Association of excessive mobile phone use during pregnancy with birth weight: an adjunct study in Kumamoto of Japan Environment and Children’s Study. Environmental Health and Preventive Medicine. 22(1). doi:10.1186/s12199-017-0656-1. http://dx.doi.org/10.1186/s12199-017-0656-1.
276. Boileau N, Margueritte F, Gauthier T, Boukeffa N, Preux P-M, Labrunie A, Aubard Y. 2020. Mobile phone use during pregnancy: Which association with fetal growth? Journal of Gynecology Obstetrics and Human Reproduction. 49(8):101852. doi:10.1016/j.jogoh.2020.101852. http://dx.doi.org/10.1016/j.jogoh.2020.101852.
277. Hutcheon JA, Riddell CA, Himes KP. 2021. A New Approach for Classifying Fetal Growth Restriction. Epidemiology. 32(6):860–867. doi:10.1097/ede.0000000000001399. http://dx.doi.org/10.1097/ede.0000000000001399.
278. Cao Y, Zhang Y, Liu Y. 2006. Effects of exposure to extremely low frequency electromagnetic fields on reproduction of female mice and development of offsprings. Zhonghua lao dong wei sheng zhi ye bing za zhi = Zhonghua laodong weisheng zhiyebing zazhi = Chinese journal of industrial hygiene and occupational diseases. 24(8):468–70. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/16978513/.
279. Sangun O, Dundar B, Darici H, Comlekci S, Doguc DK, Celik S. 2014. The effects of long-term exposure to a 2450 MHz electromagnetic field on growth and pubertal development in female Wistar rats. Electromagnetic Biology and Medicine. 34(1):63–71. doi:10.3109/15368378.2013.871619. http://dx.doi.org/10.3109/15368378.2013.871619.
280. Terrell ML, Hartnett KP, Marcus M. 2011. Can environmental or occupational hazards alter the sex ratio at birth? A systematic review. Emerging Health Threats Journal. 4(1):7109. doi:10.3402/ehtj.v4i0.7109. http://dx.doi.org/10.3402/ehtj.v4i0.7109.
281. Knave B, Gamberale F, Bergström S, Birke E, Iregren A, Kolmodin-Hedman B, Wennberg A. 1979. Long-term exposure to electric fields. A cross-sectional epidemiologic investigation of occupationally exposed workers in high-voltage substations. Scandinavian Journal of Work, Environment & Health. 5(2):115–125. doi:10.5271/sjweh.2661. http://dx.doi.org/10.5271/sjweh.2661.
282. Albanes D. 1999. β-Carotene and lung cancer: a case study. The American Journal of Clinical Nutrition. 69(6):1345S-1350S. doi:10.1093/ajcn/69.6.1345s. http://dx.doi.org/10.1093/ajcn/69.6.1345s.
283. Poston L, Briley A, Seed P, Kelly F, Shennan A. 2006. Vitamin C and vitamin E in pregnant women at risk for pre-eclampsia (VIP trial): randomised placebo-controlled trial. The Lancet. 367(9517):1145–1154. doi:10.1016/s0140-6736(06)68433-x. http://dx.doi.org/10.1016/s0140-6736(06)68433-x.
284. Klein EA, Thompson IM, Tangen CM, Crowley JJ, Lucia MS, Goodman PJ, Minasian LM, Ford LG, Parnes HL, Gaziano JM, et al. 2011. Vitamin E and the Risk of Prostate Cancer. JAMA. 306(14):1549. doi:10.1001/jama.2011.1437. http://dx.doi.org/10.1001/jama.2011.1437.
285. Bioinitiative. 2022. Henry Lai’s Research Summaries. [accessed 2024 Mar 27]. https://bioinitiative.org/research-summaries/.
286. Environmental Health Trust. Science on Health Effects of Cell Phone and Wireless Radiation. [accessed 2024 Mar 27]. https://ehtrust.org/science/science-on-health-effects-of-cell-phone-and-wireless-radiation/.
287. Levitt BB, Lai HC, Manville AM II. 2021. Effects of non-ionizing electromagnetic fields on flora and fauna, part 1. Rising ambient EMF levels in the environment. Reviews on Environmental Health. 37(1):81–122. doi:10.1515/reveh-2021-0026. http://dx.doi.org/10.1515/reveh-2021-0026.
288. Levitt BB, Lai HC, Manville AM II. 2021. Effects of non-ionizing electromagnetic fields on flora and fauna, Part 2 impacts: how species interact with natural and man-made EMF. Reviews on Environmental Health. 37(3):327–406. doi:10.1515/reveh-2021-0050. http://dx.doi.org/10.1515/reveh-2021-0050.
289. Levitt BB, Lai HC, Manville AM II. 2021. Effects of non-ionizing electromagnetic fields on flora and fauna, Part 3. Exposure standards, public policy, laws, and future directions. Reviews on Environmental Health. 37(4):531–558. doi:10.1515/reveh-2021-0083. http://dx.doi.org/10.1515/reveh-2021-0083.
290. CDC Stacks. The State of childhood asthma; United States, 1980-2005. [accessed 2023 Nov 18]. https://stacks.cdc.gov/view/cdc/6793.
291. Statistics of Japan. School Health Survey. [accessed 2023 Nov 19]. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00400002&tstat=000001011648.
292. CDC USDSS. United States Diabetes Surveillance System. [accessed 2023 Nov 18]. https://gis.cdc.gov/grasp/diabetes/diabetesatlas.html.
293. Sasamori H, Takahashi E, Nakagawa T, Matsuki T. 2015. 2014 nen Ningen Dock Zenkoku Syuukei Seiseki Houkoku (2014 national aggregate results report for comprehensive medical checkups). Ningen Dock. 30(4):750–762. https://doi.org/10.11320/ningendock.30.750.
294. Keenan T, Rosen P, Yeates D, Goldacre M. 2007. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. British Journal of Ophthalmology. 91(7):901–904. doi:10.1136/bjo.2006.108977. http://dx.doi.org/10.1136/bjo.2006.108977.
295. Savitz DA, Liao D, Sastre A, Kleckner RC, Kavet R. 1999. Magnetic Field Exposure and Cardiovascular Disease Mortality among Electric Utility Workers. American Journal of Epidemiology. 149(2):135–142. doi:10.1093/oxfordjournals.aje.a009779. http://dx.doi.org/10.1093/oxfordjournals.aje.a009779.
296. Tikhonova GI. 2003. Epidemiological risk assessment of pathology development in occupational exposure to radiofrequency electromagnetic fields. Radiatsionnaia biologiia, radioecologiia. 43(5):559–64. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/14658291/.
297. Sahl J. 2002. Occupational Magnetic Field Exposure and Cardiovascular Mortality in a Cohort of Electric Utility Workers. American Journal of Epidemiology. 156(10):913–918. doi:10.1093/aje/kwf076. http://dx.doi.org/10.1093/aje/kwf076.
298. Hakansson N. 2003. Occupational Exposure to Extremely Low Frequency Magnetic Fields and Mortality from Cardiovascular Disease. American Journal of Epidemiology. 158(6):534–542. doi:10.1093/aje/kwg197. http://dx.doi.org/10.1093/aje/kwg197.
299. Wilén J, Hörnsten R, Sandström M, Bjerle P, Wiklund U, Stensson O, Lyskov E, Mild KH. 2003. Electromagnetic field exposure and health among RF plastic sealer operators. Bioelectromagnetics. 25(1):5–15. doi:10.1002/bem.10154. http://dx.doi.org/10.1002/bem.10154.
300. Déoux S, Déoux P, Szabason F. 1997. Occupational So-Hz Magnetic Field Exposure and Human Heart Rate: A Case Report. Electro- and Magnetobiology. 16(2):153–159. doi:10.3109/15368379709009840. http://dx.doi.org/10.3109/15368379709009840.
301. Kilicalp D, Deger Y, Çınar A. 2009. Effects of Green Tea on Electrocardiography of Guinea Pigs Exposed to Electromagnetic Field Emitted by Mobile Phones. Kafkas Universitesi Veteriner Fakultesi Dergisi. 15(6):823–828. https://www.researchgate.net/publication/273030017.
302. Piek A, de Boer RA, Silljé HHW. 2016. The fibrosis-cell death axis in heart failure. Heart Failure Reviews. 21(2):199–211. doi:10.1007/s10741-016-9536-9. http://dx.doi.org/10.1007/s10741-016-9536-9.
303. Piek A, de Boer RA, Silljé HHW. 2016. The fibrosis-cell death axis in heart failure. Heart Failure Reviews. 21(2):199–211. doi:10.1007/s10741-016-9536-9. http://dx.doi.org/10.1007/s10741-016-9536-9.
304. Kazbanov IV, ten Tusscher KHWJ, Panfilov AV. 2016. Effects of Heterogeneous Diffuse Fibrosis on Arrhythmia Dynamics and Mechanism. Scientific Reports. 6(1). doi:10.1038/srep20835. http://dx.doi.org/10.1038/srep20835.
305. Verheule S, Schotten U. 2021. Electrophysiological Consequences of Cardiac Fibrosis. Cells. 10(11):3220. doi:10.3390/cells10113220. http://dx.doi.org/10.3390/cells10113220.
306. Liu YQ, Gao YB, Dong J, Yao BW, Zhao L, Peng RY. 2015. Pathological changes in the sinoatrial node tissues of rats caused by pulsed microwave exposure. Biomedical and environmental sciences : BES. 28(1):72–5. doi:10.3967/bes2015.007. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/25566864/.
307. Bozza PT, Viola JPB. 2010. Lipid droplets in inflammation and cancer. Prostaglandins, Leukotrienes and Essential Fatty Acids (PLEFA). 82(4–6):243–250. doi:10.1016/j.plefa.2010.02.005. http://dx.doi.org/10.1016/j.plefa.2010.02.005.
308. Kiray A, Tayefi H, Kiray M, Bagriyanik HA, Pekcetin C, Ergur BU, Ozogul C. 2012. The effects of exposure to electromagnetic field on rat myocardium. Toxicology and Industrial Health. 29(5):418–425. doi:10.1177/0748233711434957. http://dx.doi.org/10.1177/0748233711434957.
309. Türedi S, Hancı H, Topal Z, Ünal D, Mercantepe T, Bozkurt İ, Kaya H, Odacı E. 2014. The effects of prenatal exposure to a 900-MHz electromagnetic field on the 21-day-old male rat heart. Electromagnetic Biology and Medicine. 34(4):390–397. doi:10.3109/15368378.2014.952742. http://dx.doi.org/10.3109/15368378.2014.952742.
310. Milham S Jr. 1985. Mortality in workers exposed to electromagnetic fields. Environmental Health Perspectives. 62:297–300. doi:10.1289/ehp.8562297. http://dx.doi.org/10.1289/ehp.8562297.
311. Li D-K. 2011. Maternal Exposure to Magnetic Fields During Pregnancy in Relation to the Risk of Asthma in Offspring. Archives of Pediatrics & Adolescent Medicine. 165(10):945. doi:10.1001/archpediatrics.2011.135. http://dx.doi.org/10.1001/archpediatrics.2011.135.
312. Booth RJ, Beale IL, Heriot SA, Pearce NE. 2001. Association of health problems with 50 Hz magnetic fields in human adults living near power transmission lines. Journal of the Australasian College of Nutritional and Environmental Medicine. 20(2). https://search.informit.org/doi/abs/10.3316/INFORMIT.542337929245324.
313. Bush A. 2008. COPD: A Pediatric Disease. COPD: Journal of Chronic Obstructive Pulmonary Disease. 5(1):53–67. doi:10.1080/15412550701815965. http://dx.doi.org/10.1080/15412550701815965.
314. Gibson PG, Simpson JL. 2009. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 64(8):728–735. doi:10.1136/thx.2008.108027. http://dx.doi.org/10.1136/thx.2008.108027.
315. Bisgaard H, Jensen SM, Bønnelykke K. 2012. Interaction between Asthma and Lung Function Growth in Early Life. American Journal of Respiratory and Critical Care Medicine. 185(11):1183–1189. doi:10.1164/rccm.201110-1922oc. http://dx.doi.org/10.1164/rccm.201110-1922oc.
316. Yahyazadeh A, Kıvrak EG, Koç GE. 2021. Protective effect of melatonin on the rat lung following exposure to 900-MHz electromagnetic field: a stereological and histopathological study. Journal of Experimental and Clinical Medicine. 38(2):55–60. doi:10.52142/omujecm.38.2.1. http://dx.doi.org/10.52142/omujecm.38.2.1.
317. Gharib OA. 2011. Role of Kombucha Tea in the Control of EMF 950 MHz Induced Injury in Rat Heart and Lung Organs. Asian Journal of Pharmaceutical and Biological. 1(3):281–288. https://www.researchgate.net/publication/232282167/.
318. Baltaci AK, Mogulkoc R, Salbacak A, Celik I, Sivrikaya A. 2012. The role of zinc supplementation in the inhibition of tissue damage caused by exposure to electromagnetic field in rat lung and liver tissues. Bratislava Medical Journal. 113(07):400–403. doi:10.4149/bll_2012_090. http://dx.doi.org/10.4149/bll_2012_090.
319. Meo S, Alsubaie Y, Almubarak Z, Almutawa H, AlQasem Y, Hasanato R. 2015. Association of Exposure to Radio-Frequency Electromagnetic Field Radiation (RF-EMFR) Generated by Mobile Phone Base Stations with Glycated Hemoglobin (HbA1c) and Risk of Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health. 12(11):14519–14528. doi:10.3390/ijerph121114519. http://dx.doi.org/10.3390/ijerph121114519.
320. Cnop M, Welsh N, Jonas J-C, Jörns A, Lenzen S, Eizirik DL. 2005. Mechanisms of Pancreatic β-Cell Death in Type 1 and Type 2 Diabetes. Diabetes. 54(suppl_2):S97–S107. doi:10.2337/diabetes.54.suppl_2.s97. http://dx.doi.org/10.2337/diabetes.54.suppl_2.s97.
321. Tsuruzoe K, Nishikawa T, Araki E. 2006. Sanka Stress to Insulin Teikousei (Oxidative Stress and Insulin Resistance). Tounyoubyou (Diabetes). 49(11):845–848. https://doi.org/10.11213/tonyobyo.49.845.
322. Mukherjee B, Hossain CM, Mondal L, Paul P, Ghosh MK. 2013. Obesity and Insulin Resistance: An Abridged Molecular Correlation. Lipid Insights. 6:LPI.S10805. doi:10.4137/lpi.s10805. http://dx.doi.org/10.4137/lpi.s10805.
323. Khaki AA, Ali-Hemmati A, Nobahari R. 2015. A Study of the Effects of Electromagnetic Field on Islets of Langerhans and Insulin Release in Rats. Crescent Journal of Medical and Biological Sciences. 2(1):1–5. https://www.academia.edu/85097507.
324. Bahaoddini A, Mohabatkar H, Nikfarjam A, Keshtgar S. 2008. Effect of Exposure to Low Frequency Electromagnetic Field on the Plasma Glucose, Insulin, Triglyceride and Cholesterol of Male Rats. Journal of Applied Animal Research. 34(2):179–180. doi:10.1080/09712119.2008.9706966. http://dx.doi.org/10.1080/09712119.2008.9706966.
325. Masoumi A, Karbalaei N, Mortazavi SMJ, Shabani M. 2018. Radiofrequency radiation emitted from Wi-Fi (2.4 GHz) causes impaired insulin secretion and increased oxidative stress in rat pancreatic islets. International Journal of Radiation Biology. 94(9):850–857. doi:10.1080/09553002.2018.1490039. http://dx.doi.org/10.1080/09553002.2018.1490039.
326. Meo S, Rubeaan K. 2013. Effects of exposure to electromagnetic field radiation (EMFR) generated by activated mobile phones on fasting blood glucose. International Journal of Occupational Medicine and Environmental Health. 26(2). doi:10.2478/s13382-013-0107-1. http://dx.doi.org/10.2478/s13382-013-0107-1.
327. Ebrahimzadeh E, Pooyan M, Bijar A. 2014. A Novel Approach to Predict Sudden Cardiac Death (SCD) Using Nonlinear and Time-Frequency Analyses from HRV Signals. Talkachova A, editor. PLoS ONE. 9(2):e81896. doi:10.1371/journal.pone.0081896. http://dx.doi.org/10.1371/journal.pone.0081896.
328. Xhyheri B, Manfrini O, Mazzolini M, Pizzi C, Bugiardini R. 2012. Heart Rate Variability Today. Progress in Cardiovascular Diseases. 55(3):321–331. doi:10.1016/j.pcad.2012.09.001. http://dx.doi.org/10.1016/j.pcad.2012.09.001.
329. Shaffer F, Ginsberg JP. 2017. An Overview of Heart Rate Variability Metrics and Norms. Frontiers in Public Health. 5. doi:10.3389/fpubh.2017.00258. http://dx.doi.org/10.3389/fpubh.2017.00258.
330. Bortkiewicz A, Gadzicka E, Zmyślony M, Szymczak W. 2006. Neurovegetative disturbances in workers exposed to 50 Hz electromagnetic fields. International journal of occupational medicine and environmental health. 19(1):53–60. doi:10.2478/v10001-006-0001-1. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/16881599/.
331. Bortkiewicz A, Gadzicka E, Szymczak W, Zmyślony M. 2012. Heart rate variability (HRV) analysis in radio and TV broadcasting stations workers. International journal of occupational medicine and environmental health. 25(4):446–55. doi:10.2478/s13382-012-0059-x. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/23224733/.
332. Bellieni CV, Acampa M, Maffei M, Maffei S, Perrone S, Pinto I, Stacchini N, Buonocore G. 2007. Electromagnetic fields produced by incubators influence heart rate variability in newborns. Archives of Disease in Childhood - Fetal and Neonatal Edition. 93(4):F298–F301. doi:10.1136/adc.2007.132738. http://dx.doi.org/10.1136/adc.2007.132738.
333. Baldi E, Baldi C, Lithgow BJ. 2006. A pilot investigation of the effect of extremely low frequency pulsed electromagnetic fields on humans’ heart rate variability. Bioelectromagnetics. 28(1):64–68. doi:10.1002/bem.20268. http://dx.doi.org/10.1002/bem.20268.
334. Parazzini M, Ravazzani P, Tognola G, Thuróczy G, Molnar FB, Sacchettini A, Ardesi G, Mainardi LT. 2006. Electromagnetic fields produced by GSM cellular phones and heart rate variability. Bioelectromagnetics. 28(2):122–129. doi:10.1002/bem.20275. http://dx.doi.org/10.1002/bem.20275.
335. Dauda Usman J, Umar Isyaku M, Fasanmade AA. 2020. Evaluation of heart rate variability, blood pressure and lipid profile alterations from dual transceiver mobile phone radiation exposure. Journal of Basic and Clinical Physiology and Pharmacology. 32(5):951–957. doi:10.1515/jbcpp-2020-0047. http://dx.doi.org/10.1515/jbcpp-2020-0047.
336. Wieling W, van Brederode JFM, de Rijk LG, Borst C, Dunning AJ. 1982. Reflex control of heart rate in normal subjects in relation to age: A data base for cardiac vagal neuropathy. Diabetologia. 22(3):163–166. doi:10.1007/bf00283745. http://dx.doi.org/10.1007/bf00283745.
337. Singer DH, Martin GJ, Magid N, Weiss JS, Schaad JW, Kehoe R, Zheutlin T, Fintel DJ, Hsieh A-M, Lesch M. 1988. Low heart rate variability and sudden cardiac death. Journal of Electrocardiology. 21:S46–S55. doi:10.1016/0022-0736(88)90055-6. http://dx.doi.org/10.1016/0022-0736(88)90055-6.
338. Shen MJ, Zipes DP. 2014. Role of the Autonomic Nervous System in Modulating Cardiac Arrhythmias. Circulation Research. 114(6):1004–1021. doi:10.1161/circresaha.113.302549. http://dx.doi.org/10.1161/circresaha.113.302549.
339. Franco P, Szliwowski H, Dramaix M, Kahn A. 1999. Decreased Autonomic Responses to Obstructive Sleep Events in Future Victims of Sudden Infant Death Syndrome. Pediatric Research. 46(1):33–39. doi:10.1203/00006450-199907000-00006. http://dx.doi.org/10.1203/00006450-199907000-00006.
340. Liao D, Cai J, Brancati FL, Folsom A, Barnes RW, Tyroler HA, Heiss G. 1995. Association of vagal tone with serum insulin, glucose, and diabetes mellitus — The ARIC Study. Diabetes Research and Clinical Practice. 30(3):211–221. doi:10.1016/0168-8227(95)01190-0. http://dx.doi.org/10.1016/0168-8227(95)01190-0.
341. Koschke M, Boettger MK, Schulz S, Berger S, Terhaar J, Voss A, Yeragani VK, Bär K-J. 2009. Autonomy of Autonomic Dysfunction in Major Depression. Psychosomatic Medicine. 71(8):852–860. doi:10.1097/psy.0b013e3181b8bb7a. http://dx.doi.org/10.1097/psy.0b013e3181b8bb7a.
342. Jarrett ME, Burr RL, Cain KC, Hertig V, Weisman P, Heitkemper MM. 2003. Digestive Diseases and Sciences. 48(2):386–394. doi:10.1023/a:1021904216312. http://dx.doi.org/10.1023/a:1021904216312.
343. Liu Xin, Zhao L, Yu D, Ma S, Liu Xiaodong. 2013. Effects of extremely low frequency electromagnetic field on the health of workers in automotive industry. Electromagnetic Biology and Medicine. 32(4):551–559. doi:10.3109/15368378.2013.773909. http://dx.doi.org/10.3109/15368378.2013.773909.
344. Aziz IA, Elwasife K, Abujami M, Shabat M, Shahwan U. 2017. Analysis of the Biochemical Parameters of Liver, Kidney Functions and Thyroid Stimulated Hormone in Children after Exposure to Mobile Phone Base Station Radiation and Therapeutic Action of Olive Oil. IUG Journal of Natural Studies.:79–84. https://www.researchgate.net/publication/315729021.
345. Peighambarzadeh SA, Tavana M. 2017. Effects of electromagnetic field radiation on biochemical parameters in swiss albino mice. Banat’s Journal of Biotechnology. 8(16):48–53. https://www.researchgate.net/publication/320956051.
346. Shoorei H, Seghinsara AM, Abedelahi A. 2018. Protective Effects of Vitamin E and Selenium on Liver Tissue Damages Induced by Electromagnetic Field: An Ultrastructural Study. Crescent Journal of Medical and Biological Sciences. 5(4):338–344. https://www.researchgate.net/publication/324569912.
347. TOPAL Z, HANCI H, MERCANTEPE T, EROL HS, KELEŞ ON, KAYA H, MUNGAN S, ODACI E. 2015. The effects of prenatal long-duration exposure to 900-MHz electromagnetic field on the 21-day-old newborn male rat liver. TURKISH JOURNAL OF MEDICAL SCIENCES. 45:291–297. doi:10.3906/sag-1404-168. http://dx.doi.org/10.3906/sag-1404-168.
348. Miller MA, Zachary JF. 2017. Mechanisms and Morphology of Cellular Injury, Adaptation, and Death. Pathologic Basis of Veterinary Disease.:2-43.e19. doi:10.1016/b978-0-323-35775-3.00001-1. http://dx.doi.org/10.1016/b978-0-323-35775-3.00001-1.
349. Bedir R, Tumkaya L, Mercantepe T, Yilmaz A. 2018. Pathological Findings Observed in the Kidneys of Postnatal Male Rats Exposed to the 2100 MHz Electromagnetic Field. Archives of Medical Research. 49(7):432–440. doi:10.1016/j.arcmed.2018.12.010. http://dx.doi.org/10.1016/j.arcmed.2018.12.010.
350. Eddy AA. 2014. Overview of the cellular and molecular basis of kidney fibrosis. Kidney International Supplements. 4(1):2–8. doi:10.1038/kisup.2014.2. http://dx.doi.org/10.1038/kisup.2014.2.
351. Hanif MO, Bali A, Ramphul K. 2023. Acute Renal Tubular Necrosis. In: StatPearls. Treasure Island (FL): StatPearls Publishing. [accessed 2024 Feb 6]. https://pubmed.ncbi.nlm.nih.gov/29939592/.
352. Oktem F, Ozguner F, Mollaoglu H, Koyu A, Uz E. 2005. Oxidative Damage in the Kidney Induced by 900-MHz-Emitted Mobile Phone: Protection by Melatonin. Archives of Medical Research. 36(4):350–355. doi:10.1016/j.arcmed.2005.03.021. http://dx.doi.org/10.1016/j.arcmed.2005.03.021.
353. Vinson JA. 2006. Oxidative stress in cataracts. Pathophysiology. 13(3):151–162. doi:10.1016/j.pathophys.2006.05.006. http://dx.doi.org/10.1016/j.pathophys.2006.05.006.
354. AURELL E, TENGROTH B. 1973. LENTICULAR AND RETINAL CHANGES SECONDARY TO MICROWAVE EXPOSURE. Acta Ophthalmologica. 51(6):764–771. doi:10.1111/j.1755-3768.1973.tb06045.x. http://dx.doi.org/10.1111/j.1755-3768.1973.tb06045.x.
355. Hässig M, Jud F, Spiess B. 2012. Vermehrtes Auftreten von nukleärer Katarakt beim Kalb nach Erstellung einer Mobilfunkbasisstation. Schweizer Archiv für Tierheilkunde. 154(2):82–86. doi:10.1024/0036-7281/a000300. http://dx.doi.org/10.1024/0036-7281/a000300.
356. Balci M, Devrim E, Durak I. 2007. Effects of Mobile Phones on Oxidant/Antioxidant Balance in Cornea and Lens of Rats. Current Eye Research. 32(1):21–25. doi:10.1080/02713680601114948. http://dx.doi.org/10.1080/02713680601114948.
357. Phillips JL, Rutledge L, Winters WD. 1986. Transferrin binding to two human colon carcinoma cell lines: characterization and effect of 60-Hz electromagnetic fields. Cancer research. 46(1):239–44. [accessed 2024 Mar 27]. https://pubmed.ncbi.nlm.nih.gov/2998606/.
358. Hore PJ, Mouritsen H. 2016. The Radical-Pair Mechanism of Magnetoreception. Annual Review of Biophysics. 45(1):299–344. doi:10.1146/annurev-biophys-032116-094545. http://dx.doi.org/10.1146/annurev-biophys-032116-094545.
359. Ritz T, Wiltschko R, Hore PJ, Rodgers CT, Stapput K, Thalau P, Timmel CR, Wiltschko W. 2009. Magnetic Compass of Birds Is Based on a Molecule with Optimal Directional Sensitivity. Biophysical Journal. 96(8):3451–3457. doi:10.1016/j.bpj.2008.11.072. http://dx.doi.org/10.1016/j.bpj.2008.11.072.
360. Vácha M, Půžová T, Kvíćalová M. 2009. Radio frequency magnetic fields disrupt magnetoreception in American cockroach. Journal of Experimental Biology. 212(21):3473–3477. doi:10.1242/jeb.028670. http://dx.doi.org/10.1242/jeb.028670.
361. Müller P, Ahmad M. 2011. Light-activated Cryptochrome Reacts with Molecular Oxygen to Form a Flavin–Superoxide Radical Pair Consistent with Magnetoreception. Journal of Biological Chemistry. 286(24):21033–21040. doi:10.1074/jbc.m111.228940. http://dx.doi.org/10.1074/jbc.m111.228940.
362. Sherrard RM, Morellini N, Jourdan N, El-Esawi M, Arthaut L-D, Niessner C, Rouyer F, Klarsfeld A, Doulazmi M, Witczak J, et al. 2018. Low-intensity electromagnetic fields induce human cryptochrome to modulate intracellular reactive oxygen species. Keays D, editor. PLOS Biology. 16(10):e2006229. doi:10.1371/journal.pbio.2006229. http://dx.doi.org/10.1371/journal.pbio.2006229.
363. Barnes FS, Greenebaum B. 2014. The effects of weak magnetic fields on radical pairs. Bioelectromagnetics. 36(1):45–54. doi:10.1002/bem.21883. http://dx.doi.org/10.1002/bem.21883.
364. Mohawk JA, Green CB, Takahashi JS. 2012. Central and Peripheral Circadian Clocks in Mammals. Annual Review of Neuroscience. 35(1):445–462. doi:10.1146/annurev-neuro-060909-153128. http://dx.doi.org/10.1146/annurev-neuro-060909-153128.
365. Gauger J. 1985. Household Appliance Magnetic Field Survey. IEEE Transactions on Power Apparatus and Systems. PAS-104(9):2435–2444. doi:10.1109/tpas.1985.318988. http://dx.doi.org/10.1109/tpas.1985.318988.
366. Aerts S, Calderon C, Valič B, Maslanyj M, Addison D, Mee T, Goiceanu C, Verloock L, Van den Bossche M, Gajšek P, et al. 2017. Measurements of intermediate-frequency electric and magnetic fields in households. Environmental Research. 154:160–170. doi:10.1016/j.envres.2017.01.001. http://dx.doi.org/10.1016/j.envres.2017.01.001.
367. Florig HK, Hoburg JF. Power-frequency magnetic fields from electric blankets. In: Images of the Twenty-First Century. Proceedings of the Annual International Engineering in Medicine and Biology Society. IEEE. http://dx.doi.org/10.1109/iembs.1989.96141.
368. Tell RA, Kavet R. 2016. ELECTRIC AND MAGNETIC FIELDS <100 KHZ IN ELECTRIC AND GASOLINE-POWERED VEHICLES. Radiation Protection Dosimetry. 172(4):541–546. doi:10.1093/rpd/ncv533. http://dx.doi.org/10.1093/rpd/ncv533.
369. Japan EMF Information Center. Mi no Mawari no Hassei-gen (densya) (Sources Around You (trains)) . [accessed 2023 Aug 8]. https://www.jeic-emf.jp/public/story/around/railroad.html.
370. Marinescu IE, Poparlan C. 2016. Assessment of GSM HF-Radiation Impact Levels within the Residential Area of Craiova City. Procedia Environmental Sciences. 32:177–183. doi:10.1016/j.proenv.2016.03.022. http://dx.doi.org/10.1016/j.proenv.2016.03.022.
371. Al-Ruwais AS. 2001. Measurements of RF Radiation in the Vicinity of FM and TV Broadcasting Stations. Sultan Qaboos University Journal for Science [SQUJS]. 6(1):45. doi:10.24200/squjs.vol6iss1pp45-51. http://dx.doi.org/10.24200/squjs.vol6iss1pp45-51.
372. Thompson DF. 1993. Understanding Financial Conflicts of Interest. New England Journal of Medicine. 329(8):573–576. doi:10.1056/nejm199308193290812. http://dx.doi.org/10.1056/nejm199308193290812.
373. Becker R. 1998. The Body Electric: Electromagnetism And The Foundation Of Life. [accessed 2024 Mar 27]. https://www.google.co.jp/books/edition/The_Body_Electric/q-6Rdjs0h-wC?hl=en.
374. Environmental Health Trust. EHT Wins in Historic Decision, Federal Court Orders FCC to Explain Why It Ignored Scientific Evidence Showing Harm from Wireless Radiation. [accessed 2024 Mar 28]. https://ehtrust.org/in-historic-decision-federal-court-finds-fcc-failed-to-explain-why-it-ignored-scientific-evidence-showing-harm-from-wireless-radiation/.
375. Davis DL. 2015. The truth about mobile phone and wireless radiation. [accessed 2023 Jul 17]. https://www.youtube.com/watch?v=BwyDCHf5iCY.
376. Brandt AM. 2012. Inventing Conflicts of Interest: A History of Tobacco Industry Tactics. American Journal of Public Health. 102(1):63–71. doi:10.2105/ajph.2011.300292. http://dx.doi.org/10.2105/ajph.2011.300292.